Most people think COPD is caused by smoking. And while that’s true for the majority, there’s another cause many doctors miss - one that’s genetic, often shows up before age 45, and can run in families. It’s called Alpha-1 Antitrypsin Deficiency, or AATD. If you’ve been told you have COPD but never smoked, or if your symptoms started young, this might be the real reason behind your breathing problems.
What Is Alpha-1 Antitrypsin Deficiency?
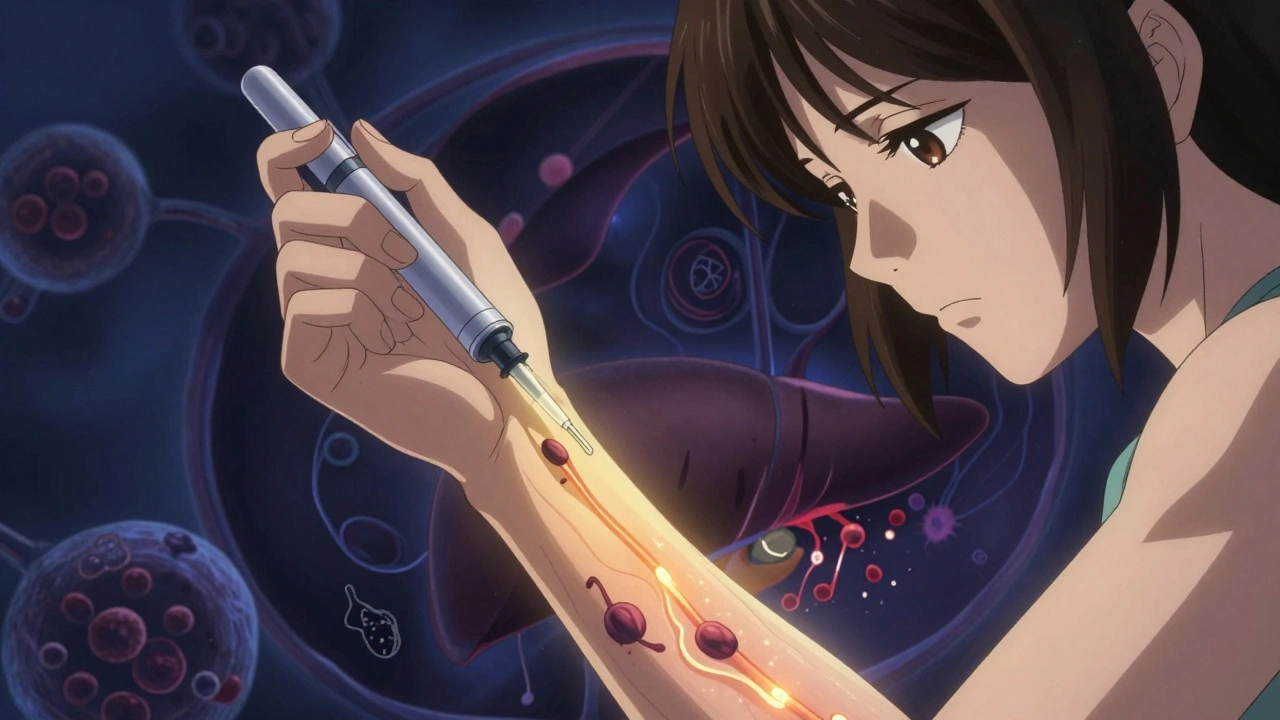
Alpha-1 antitrypsin (AAT) is a protein made in your liver. Its job? To protect your lungs from damage caused by white blood cells called neutrophils. These cells fight infection, but they also release an enzyme - neutrophil elastase - that can break down lung tissue if left unchecked. AAT acts like a shield, stopping that enzyme from tearing up your air sacs.
In AATD, a faulty gene - called SERPINA1 - tells your liver to make a broken version of this protein. Instead of flowing out into your bloodstream, the bad protein clumps up inside liver cells. That means your lungs don’t get enough protection. Over time, your lungs start to break down, leading to emphysema - a type of COPD. At the same time, the clumped protein damages your liver, sometimes causing cirrhosis or even liver cancer.
This isn’t rare. About 1 in 2,000 to 1 in 5,000 people have it. But here’s the problem: 90% of them don’t know it. Most get diagnosed after years of being told they have asthma or "smoker’s lung," even if they never smoked.
How Do You Get It?
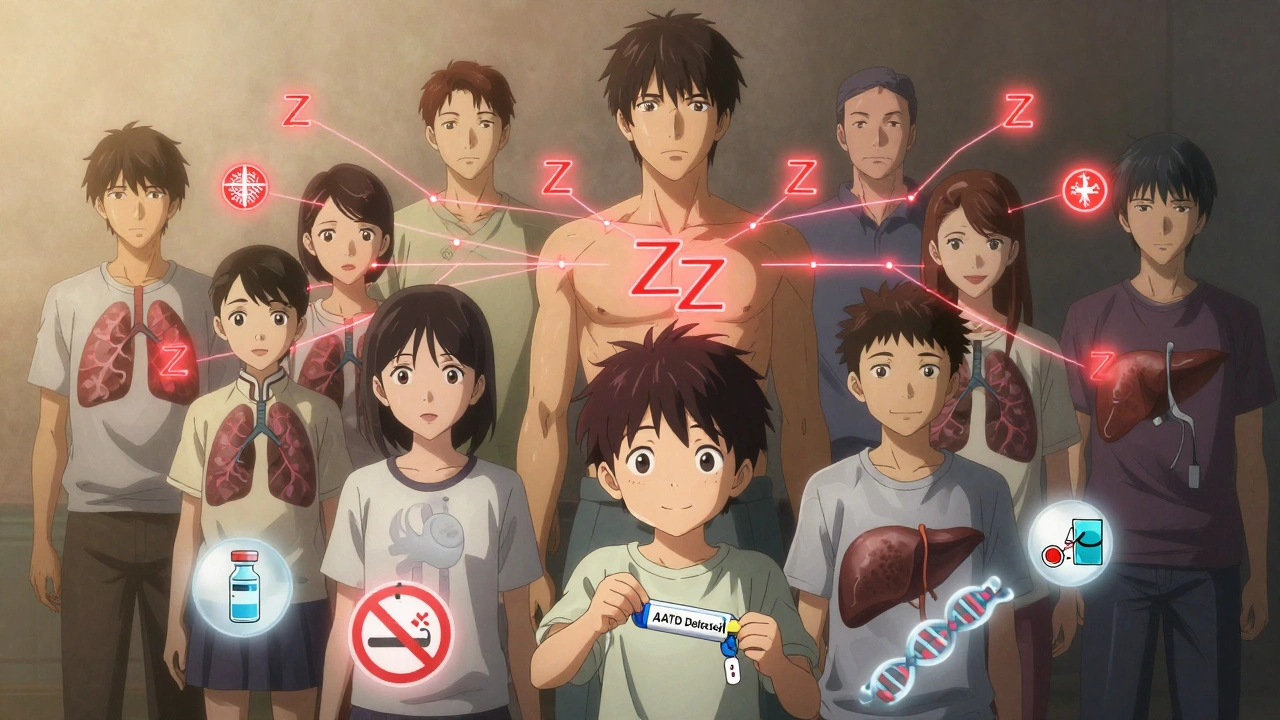
AATD is inherited. You get one copy of the gene from each parent. The normal version is called M. The two main bad versions are S and Z.
- MM = Normal. No risk.
- MZ = Carrier. Usually no symptoms, but smoking increases lung damage risk.
- SS = Mild deficiency. Some risk of lung or liver issues.
- ZZ = Severe deficiency. High risk of early COPD and liver disease.
People with ZZ genotype have only 10-20% of normal AAT levels. That’s not enough to protect the lungs. Studies show they have a 75% lifetime chance of developing lung symptoms - especially if they smoke.
And yes, you can pass this on. If you have ZZ, every one of your children will get at least one Z gene. If your partner is a carrier (MZ), each child has a 50% chance of being ZZ.
Why Is It So Often Missed?
Doctors don’t test for it unless they think to. The American Thoracic Society says everyone with COPD should be tested. But in practice, only 1 in 10 people with AATD are diagnosed.
Why? Because the symptoms look just like regular COPD: shortness of breath, chronic cough, wheezing, frequent lung infections. The big clues that point to AATD are:
- Diagnosed before age 45
- No smoking history, or minimal exposure
- Emphysema in the lower parts of the lungs (basilar), not the top
- Family history of COPD, liver disease, or unexplained lung problems
- Unexplained liver issues in adults or children
It takes an average of 8 years and three different doctors before someone with AATD gets the right diagnosis. Many patients describe it as a "diagnostic odyssey" - going from one specialist to another, getting asthma inhalers, antibiotics, or steroids that help a little but never fix the root problem.
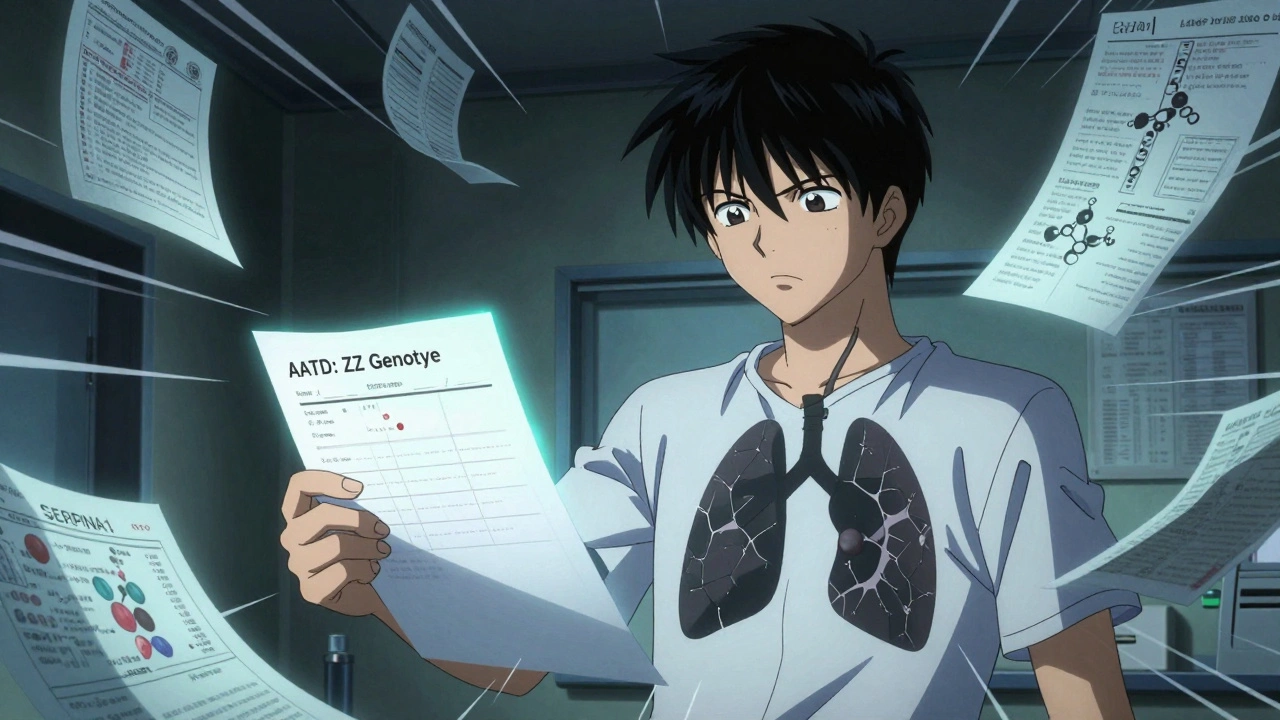
How Is It Diagnosed?
Testing is simple. First, a blood test checks your AAT level. If it’s below 11 μM (about 50 mg/dL), that’s a red flag. Then, they do a genotype test to find out which gene variants you carry - Z, S, or something rarer.
Some labs also do phenotyping, which looks at the actual shape of the protein. This helps spot unusual variants that genotyping might miss.
If you have COPD, asthma with fixed airflow blockage, unexplained liver disease, or panniculitis (a rare skin condition), you should be tested. The same goes if a close relative has AATD.
The whole process takes 2-6 weeks, depending on the lab. But once you know, you can take real steps to protect your health.
What Are the Treatment Options?
There’s no cure - yet. But there are ways to slow the damage.
1. Augmentation Therapy
This is the only treatment that replaces the missing protein. You get weekly IV infusions of purified human AAT from donor plasma. Brands include Prolastin-C, Zemaira, and Aralast NP. The goal? Keep your blood level above 11 μM - the minimum needed to protect your lungs.
Studies show this slows the loss of lung density on CT scans by up to 60% over 5 years. It doesn’t reverse damage, but it can delay the need for oxygen or transplants.
Cost? Around $70,000 to $100,000 a year. Insurance often denies it at first - you’ll need your doctor to appeal. But if you have ZZ and FEV1 between 30-65%, most insurers will cover it after paperwork.
2. Subcutaneous Therapy (Newer Option)
In 2022, the FDA approved the first subcutaneous (under-the-skin) AAT therapy: Kedrab. Instead of weekly IVs, you give yourself a shot once or twice a week. It’s less invasive, easier to manage at home, and avoids vein damage from long-term IV use.
3. Smoking Cessation - The Most Important Step
If you have AATD and you smoke, quitting is the single most effective thing you can do. Research shows it cuts your risk of severe emphysema by 60%. One patient, diagnosed at 42, quit smoking and says it added 15+ years to his life.
Even if you’ve smoked for decades, quitting at any point helps. Your lungs will still deteriorate - but slower. And you’ll reduce your risk of lung infections, heart disease, and cancer.
4. Liver Management
There’s no treatment to fix the liver damage caused by AAT clumping. But you can protect it:
- Avoid alcohol completely
- Get vaccinated for hepatitis A and B
- Don’t take unnecessary medications - especially acetaminophen (Tylenol)
- Monitor liver enzymes and ultrasound every 6-12 months
For advanced cirrhosis, a liver transplant may be needed. It’s effective - and the new liver makes normal AAT, so lung protection returns.
How Is AATD Different From Regular COPD?
| Feature | AATD-Related COPD | Smoking-Related COPD |
|---|---|---|
| Typical Age of Onset | 35-45 years | 60+ years |
| Smoking History | Often none or minimal | Usually 20+ pack-years |
| Emphysema Pattern | Lower lungs (basilar) | Upper lungs (apical) |
| Genetic Marker | Yes - SERPINA1 mutation | No |
| Specific Treatment | Augmentation therapy | Only symptom control |
| Family Risk | High - autosomal codominant | Low - environmental |
The big difference? AATD gives you a target. You know exactly what’s broken. That’s why researchers are working on gene therapy and drugs that stop the misfolded protein from clumping in the liver. These could one day treat both lung and liver damage - not just slow it.
What’s Next for AATD Treatment?
Current therapies only help the lungs. But new drugs are coming.
- Small molecule correctors - These help the faulty AAT protein fold right, so it doesn’t pile up in the liver. Early trials are promising.
- RNA interference (RNAi) - These drugs silence the bad gene in the liver, reducing toxic protein buildup. Trials are ongoing (NCT04735716, NCT05159108).
- Gene therapy - Inserting a working copy of SERPINA1 into liver cells. Still experimental, but could be a one-time fix.
By 2030, experts predict these new therapies could make up 30% of the AATD treatment market. Right now, only about 5,000 people in the U.S. get augmentation therapy - even though 25,000-30,000 have severe deficiency. That’s a huge gap.
Some states are starting newborn screening. If you’re born with ZZ, you’ll be caught early. That means you can avoid smoking, get monitored, and start treatment before lung damage begins.
What Should You Do If You Have AATD?
Here’s your action plan:
- Get tested if you have COPD, asthma with fixed obstruction, or unexplained liver disease.
- If you’re diagnosed, stop smoking - immediately. No exceptions.
- See a pulmonologist and hepatologist regularly. Get spirometry every 6-12 months.
- Ask about augmentation therapy if your FEV1 is between 30-65%.
- Get your family tested - especially siblings and children.
- Join a support group. The Alpha-1 Foundation connects patients with resources and clinical trials.
- Stay up to date on vaccines: flu, pneumonia, hepatitis.
Knowledge is power. Once you know you have AATD, you’re no longer just reacting to symptoms - you’re managing a condition with real options. And that changes everything.
Can you have Alpha-1 Antitrypsin Deficiency without ever smoking?
Yes. While smoking makes lung damage worse, AATD can cause emphysema even in lifelong non-smokers. People with the ZZ genotype often develop symptoms in their 30s or 40s without any tobacco exposure. The lack of AAT protein alone is enough to break down lung tissue over time.
Is AATD the same as cystic fibrosis?
No. Cystic fibrosis is caused by mutations in the CFTR gene and affects mucus production in the lungs, pancreas, and other organs. AATD is caused by SERPINA1 mutations and leads to low levels of a protective protein, causing lung and liver damage. Both are genetic, but they’re completely different diseases with different treatments.
Can you be a carrier and not have symptoms?
Yes. People with the MZ genotype (one normal gene, one faulty gene) usually have normal or slightly low AAT levels and rarely develop lung disease. But if they smoke, their risk of COPD increases significantly. Even without symptoms, they can pass the faulty gene to their children.
Does augmentation therapy help liver damage?
No. Augmentation therapy replaces AAT in the blood to protect the lungs, but it doesn’t reduce the toxic protein buildup in the liver. The liver damage comes from the misfolded protein clumping inside liver cells - a problem that IV infusions can’t fix. Treatments for liver disease in AATD focus on avoiding alcohol, managing complications, and, in severe cases, liver transplant.
How often do you need AAT infusions?
Standard augmentation therapy requires weekly intravenous infusions of 60 mg per kilogram of body weight. Some newer subcutaneous treatments allow dosing every 1-2 weeks. The goal is to maintain a serum AAT level above 11 μM - the minimum protective threshold. Missing doses lowers protection and increases lung damage risk.
Can children be tested for AATD?
Yes. Children with unexplained liver disease, jaundice, or elevated liver enzymes should be tested. Testing is also recommended if a parent has AATD. While lung damage doesn’t usually appear until adulthood, early detection allows families to avoid smoking, get vaccinations, and monitor liver health from childhood.

nithin Kuntumadugu
December 13, 2025 AT 20:54John Fred
December 15, 2025 AT 05:51Harriet Wollaston
December 15, 2025 AT 09:55Hamza Laassili
December 15, 2025 AT 15:49Rawlson King
December 16, 2025 AT 20:29Alvin Montanez
December 18, 2025 AT 05:23Emma Sbarge
December 19, 2025 AT 11:04Deborah Andrich
December 19, 2025 AT 14:53Sheldon Bird
December 21, 2025 AT 09:23Karen Mccullouch
December 21, 2025 AT 18:41