Imagine feeling a sharp, knife-like pain every time you go to the bathroom - not just during, but for a full hour after. That’s what an anal fissure feels like for most people. It’s not just discomfort. It’s a small tear in the lining of your anus, and if you’ve had one, you know it doesn’t go away on its own if you ignore it. About 80-90% of these tears heal within six to eight weeks with simple steps, but the other 10-20%? They turn into chronic problems that drag on for months, making sitting, walking, or even laughing painful. And here’s the thing: most people don’t realize it’s an anal fissure at first. They think it’s hemorrhoids, or a rash, or something they ate. By the time they see a doctor, they’ve already lost weeks - and sleep - to the pain.
What Exactly Is an Anal Fissure?
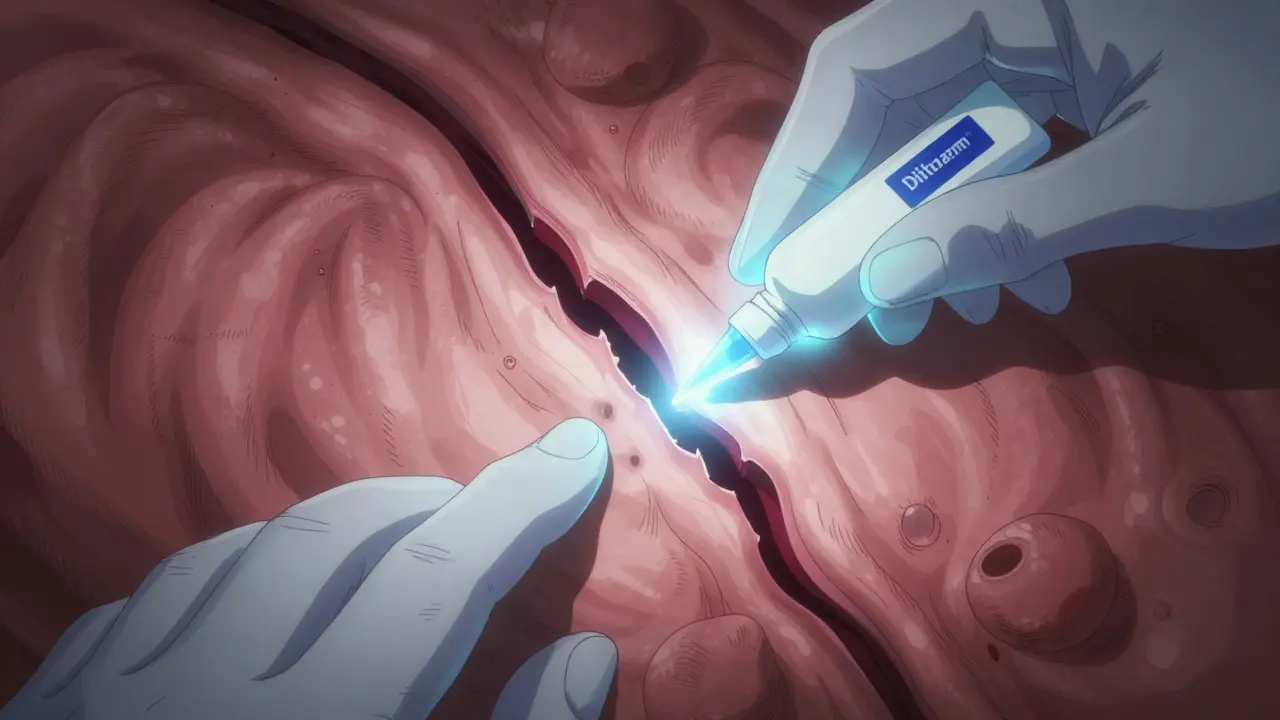
An anal fissure is a small, linear tear in the moist tissue (mucosa) that lines the anal canal. It’s not a cut you can see from the outside - it’s inside, just past the anal opening. About 90% of these tears happen in the back (posterior midline), and the other 10% show up in the front (anterior midline). That’s why doctors can often diagnose it just by asking where the pain is. The tear doesn’t heal because of a cycle that traps it in pain: when you pass a hard stool, the tear hurts. Your body reacts by clamping down the internal anal sphincter muscle to protect the area. But that muscle doesn’t relax. It stays tight, cutting off blood flow to the tear. No blood flow? No healing. And without healing, every bowel movement becomes a fresh wound.
Chronic fissures - those lasting more than eight weeks - develop their own signature look: a visible crack, a small skin tag near the opening (called a sentinel pile), and a swollen bump inside called a hypertrophied papilla. These aren’t just signs. They’re proof the body has given up on healing itself. That’s when you need to step in with more than just fiber and water.
Why Do Fissures Happen? It’s Not Just Constipation
Most people think constipation is the only cause - and yes, hard stools are the #1 trigger. But it’s not the whole story. Diarrhea can do it too. Frequent loose stools irritate the lining, making it fragile. Childbirth, anal sex, and even violent coughing or vomiting can cause tears. Babies get them too - about 64 out of every 1,000 newborns develop a fissure in their first few months. Adults between 20 and 40 are the most common group affected, with equal rates in men and women… until age 50. After that, women are three times more likely to get them, mostly because of childbirth-related trauma.
Here’s what most don’t tell you: your diet matters more than you think. The average American eats only 15 grams of fiber a day. The recommended amount? 25 to 35 grams. That’s a gap of 10 to 20 grams. That’s like trying to run a marathon with no water. Your stool gets dry, hard, and packed. It tears. And if you’ve been eating processed food, low on veggies, beans, and whole grains, you’re already setting yourself up for trouble.
How to Heal an Anal Fissure Without Surgery
Before you even think about medicine or surgery, start here. This is what works for most people, and it’s free or cheap.
- Boost your fiber intake to 30 grams a day. That’s not a suggestion - it’s the baseline. Add lentils, oats, chia seeds, apples with skin, broccoli, and pears. Don’t just add fiber - add it slowly. Jumping from 15g to 40g in one day can cause bloating and gas, which makes pain worse. Increase by 5g every 3 days until you hit 30g.
- Drink 2.5 to 3 liters of water daily. Fiber without water is like trying to mop a floor with a dry rag. It doesn’t work. Water softens stool and helps fiber do its job.
- Take sitz baths after every bowel movement. Sit in warm (not hot) water for 15 minutes. It relaxes the sphincter, increases blood flow, and cleans the area gently. Do this 3 to 4 times a day. Many people skip this because it feels silly. But 76% of NHS patients using this method saw pain drop within 72 hours.
- Use lidocaine ointment (5%) before pooping. It’s a local numbing agent. Apply a pea-sized amount inside the anus with a clean finger. It won’t heal the tear, but it stops the scream when you go.
Stick with this for at least two weeks. If you’re still in pain, it’s time to move to the next level.
Topical Medications: What Actually Works
If conservative steps don’t work after 2 weeks, it’s time for medicine. Not all ointments are created equal.
Nitroglycerin (Rectiv, 0.2-0.4%) - This is the old standard. It relaxes the sphincter muscle and boosts blood flow. But here’s the catch: 20-32% of users get bad headaches. Some people can’t tolerate it. It works in 45-68% of cases.
Diltiazem (2%) and Nifedipine (0.3%) - These are calcium channel blockers, same class as blood pressure meds. They’re gentler. Fewer headaches. Healing rates? 65-75%. The Mayo Clinic now recommends these as first-line because they’re just as effective with fewer side effects. Apply 1.25 inches of ointment on your finger, insert it 1 inch into the anus, twice a day for 8 weeks. Don’t skip doses. Missed applications are why 29% of treatments fail.
Botox injections - This isn’t for wrinkles. Injected directly into the internal sphincter, Botox paralyzes the muscle for 3-4 months. Healing rates are 50-80%. But here’s the problem: up to 40% of people get the fissure back within a year. And if it comes back, you’re back to square one - or closer to surgery.
There’s no magic bullet. But diltiazem and nifedipine are the smartest first choices. They’re safe, effective, and don’t wreck your day with headaches.
Surgery: When You’ve Run Out of Options
If you’ve tried fiber, water, sitz baths, and topical meds for 8-12 weeks with no improvement, it’s time to talk surgery. The gold standard is a lateral internal sphincterotomy. It’s a 15-20 minute procedure done under local anesthesia. The surgeon makes a tiny cut in the internal sphincter muscle to relax it permanently. Success rate? 92-98%. That’s nearly perfect.
But there’s a trade-off. About 14% of people develop minor fecal incontinence - usually just a little gas or occasional spotting. It’s not full-blown incontinence. It’s not life-changing. But it’s something you need to know before you say yes. Most patients say the trade-off is worth it. They’d rather deal with occasional leakage than live with daily knife-like pain.
Recovery? You’re back to work in 3.5 days on average. Full healing takes 6 weeks. No one says it’s easy. But compared to months of suffering? It’s a relief.
What Could Be Hiding Behind the Pain?
Not every anal pain is a fissure. Up to 10% of people diagnosed with one actually have something else - Crohn’s disease, anal cancer, sexually transmitted infections, or even tuberculosis. That’s why doctors should never assume. If you’ve had symptoms for more than 8 weeks, if you’re over 50, if you have a family history of bowel cancer, or if you’ve lost weight unexpectedly - get tested. A colonoscopy or anoscopy might be needed to rule out other causes. Don’t let a misdiagnosis delay real treatment.
What Doesn’t Work - And Why
Some things you’ve probably heard are myths:
- Wiping too hard - It doesn’t cause fissures. But it makes them worse. Use soft toilet paper or wet wipes. Or better yet - rinse with a bidet or shower.
- Using numbing creams long-term - Lidocaine helps temporarily, but it doesn’t heal. Relying on it without fixing the root cause just delays recovery.
- Going on a low-fiber diet to “rest” your bowel - That’s the opposite of what you need. Less fiber = harder stools = more tearing.
- Waiting for it to heal on its own - Acute fissures often do. Chronic ones? Almost never. The longer you wait, the more the muscle tightens, and the harder it becomes to fix.
Real Stories, Real Pain
Reddit’s r/Proctology has over 147 verified patient stories. 83% said their primary care doctor misdiagnosed them at first. One man waited 17 days before seeing a specialist. Another woman thought it was a yeast infection and used antifungal cream for three weeks. Pain didn’t go away. She finally got a diagnosis after bleeding during sex.
On the flip side, one woman in Cape Town started the 4-step plan - fiber, water, sitz baths, diltiazem. Within 10 days, her pain dropped by 70%. By 6 weeks, the tear was gone. No surgery. No Botox. Just consistency.
That’s the pattern. It’s not about fancy treatments. It’s about doing the basics right - and not giving up too soon.
What’s Next? The Future of Healing
Research is moving fast. In 2023, Johns Hopkins tested stem cell injections in 32 patients with chronic fissures that didn’t respond to anything else. After 8 weeks, 73% were healed. It’s early, but promising. The European Society of Coloproctology updated its guidelines in June 2023, now recommending diltiazem over nitroglycerin as first-line treatment. And here’s a warning: obesity and low-fiber diets are rising. Experts predict fissure cases could jump 15-20% in the next decade.
So if you’re reading this and you’re in pain - don’t wait. Start with fiber and water. Add sitz baths. Try diltiazem if it doesn’t improve. And if it’s still there after two months? See a specialist. You don’t have to live with this pain. Healing is possible. It just takes the right steps - and the will to follow through.
How long does it take for an anal fissure to heal?
Most acute anal fissures heal within 6 to 8 weeks with conservative care like fiber, fluids, and sitz baths. Chronic fissures - those lasting longer than 8 weeks - rarely heal on their own and usually require topical medications or surgery. With proper treatment, healing can occur in 4 to 12 weeks depending on the method used.
Can anal fissures come back after healing?
Yes, especially if the underlying causes aren’t addressed. Constipation, low fiber intake, and straining during bowel movements are the main reasons for recurrence. After surgery, recurrence rates are low - under 5% - if you maintain a high-fiber diet and stay hydrated. Botox treatments have higher recurrence rates, around 40%, within a year.
Is surgery the only option for chronic fissures?
No. Surgery is the most effective, but not the only option. Many people heal with topical medications like diltiazem or nifedipine, especially if they’ve been consistent with diet and sitz baths. Surgery is typically reserved for cases that don’t respond to 8-12 weeks of medical treatment. The decision should be based on your pain level, medical history, and tolerance for potential side effects like minor incontinence.
What’s the best way to prevent anal fissures?
The best prevention is consistent bowel habits. Eat 25-35 grams of fiber daily from whole grains, fruits, vegetables, and legumes. Drink 2.5-3 liters of water every day. Avoid straining. Don’t delay bowel movements. Use soft toilet paper or a bidet. If you’re prone to constipation, consider a daily psyllium supplement. Prevention is easier than treatment - and far less painful.
Can stress or anxiety cause anal fissures?
Stress doesn’t directly cause fissures, but it can worsen them. Anxiety can lead to constipation or diarrhea, both of which increase tearing risk. Stress also increases muscle tension, including in the anal sphincter, which can make healing harder. Managing stress through relaxation techniques or therapy can support recovery, but it’s not a standalone treatment.
Are anal fissures a sign of cancer?
Most anal fissures are not cancer. But in rare cases (up to 10%), symptoms that look like a fissure can be caused by anal cancer, Crohn’s disease, or other serious conditions. If you’re over 50, have unexplained weight loss, persistent bleeding, or no improvement after 8 weeks of treatment, you need further testing. Don’t assume it’s just a fissure - get it checked.
Healing from an anal fissure isn’t about quick fixes. It’s about changing habits. It’s about listening to your body when it screams during a bowel movement. It’s about choosing fiber over convenience, water over soda, and patience over impatience. You don’t need to suffer. You just need to act - and keep acting - until the pain is gone.


Sophia Daniels
December 24, 2025 AT 13:41Steven Destiny
December 25, 2025 AT 14:45Erwin Asilom
December 26, 2025 AT 20:20Brittany Fuhs
December 28, 2025 AT 14:52Peter sullen
December 28, 2025 AT 23:39Becky Baker
December 30, 2025 AT 17:32Rajni Jain
December 31, 2025 AT 20:14Natasha Sandra
January 1, 2026 AT 19:43Sumler Luu
January 2, 2026 AT 08:23sakshi nagpal
January 3, 2026 AT 00:50Sandeep Jain
January 4, 2026 AT 02:22roger dalomba
January 5, 2026 AT 03:35