Biologic therapies change how you manage chronic illness - but only if you inject them right
Biologic therapies are powerful. They’re made from living cells, not chemicals, and they target the root causes of diseases like rheumatoid arthritis, psoriasis, and Crohn’s. But they’re also fragile. One wrong move during injection - a dirty finger, a shaky hand, a rushed step - can turn a life-changing treatment into a source of infection, pain, or even hospitalization.
Most patients get these drugs at home. No clinic visits. No nurses. Just you, a pen-like injector, and a vial of medicine. And that’s where things go wrong.
A 2022 study found that nearly one-third of patients received no formal training before starting biologic injections. Others got a 30-minute demo and were sent home with six months of medication. No practice. No follow-up. No safety net.
That’s not just careless - it’s dangerous. Improper injection technique increases the risk of skin and soft tissue infections by 37%. And infections from self-injections are rising. The CDC says 12.7% of all outpatient injection-related infections come from patients who didn’t follow basic sterile practices.
What you need to know before you even touch the injector
Biologics aren’t like insulin or penicillin. They’re large molecules that can break down if mishandled. They must be kept cold. They must be used within a short window after removal from the fridge. And they must be injected into clean skin, with clean hands, using the right technique.
Before you start, make sure you have:
- A clean, well-lit space - no kitchen counters with crumbs, no beds with dirty sheets
- Soap and running water - handwashing isn’t optional. CDC says 20 seconds, scrubbing all surfaces
- Alcohol wipes - not just any wipes. Use sterile, single-use ones
- A sharps container - never throw needles in the trash
- Your medication - check the expiration date and color. If it’s cloudy or has particles, don’t use it
Many patients skip these basics because they’re in a hurry. But rushing is the #1 reason injections go wrong. Take five minutes to prepare. It saves you days of infection.
The three-step training method most patients never get
Good training isn’t a lecture. It’s not a video you watch once. It’s not a pamphlet you toss in a drawer.
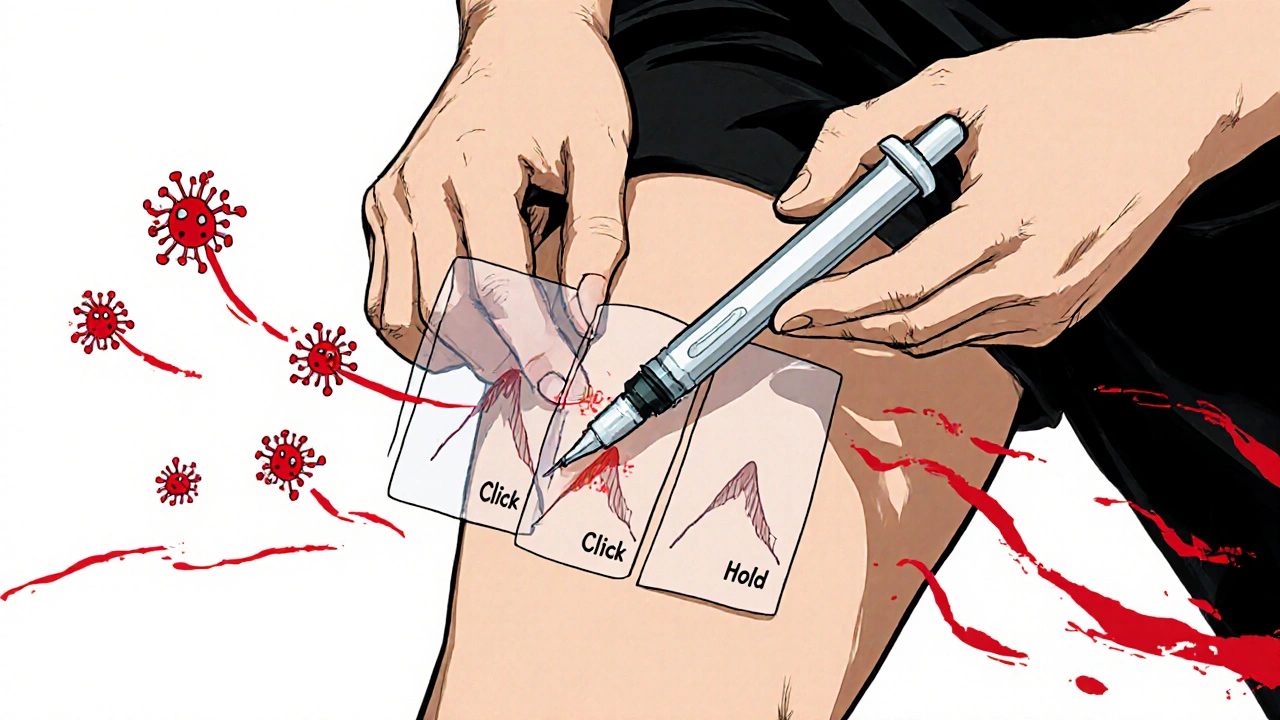
Effective training follows a simple three-step rule: Tell, Show, Do.
- Tell - Your provider explains each step: where to inject, how to hold the pen, how to click it, how long to hold it down
- Show - They demonstrate on a training device. Not the real one. A plastic replica that feels the same, but has no medicine
- Do - You do it. Right there. With supervision. They watch your grip, your pinch, your timing
Only 27% of patients in one study got all three steps. Most got only “tell.” That’s not training. That’s a warning.
If your provider skips “Do,” ask for it. Insist. If they refuse, ask for a referral to a pharmacist or nurse who specializes in injection training. Pharmacists are trained in this. They’re not just dispensing pills - they’re teaching safe delivery.
Where infections happen - and how to stop them
Infection doesn’t come from the medicine. It comes from your skin, your fingers, or your environment.
Here’s how it happens:
- You inject near a scar, a mole, or a bruise - bacteria hide there
- You wipe the skin with an alcohol wipe, then touch it with your finger to hold the skin
- You don’t wait for the alcohol to dry - moisture pulls bacteria into the puncture
- You reuse a wipe or use a dirty one
- You inject in the same spot too often - skin breaks down, bacteria builds up
Here’s how to stop it:
- Always rotate injection sites - thigh, abdomen, upper arm. Leave at least one inch between each new injection
- Wipe the skin with a fresh alcohol wipe. Let it air dry for 10 seconds. Don’t blow on it. Don’t fan it. Don’t touch it
- Don’t use your fingers to hold the skin. Use your thumb and forefinger to pinch it gently
- If you feel pain, burning, or see redness bigger than a quarter, stop. Call your doctor
- Check for fever. A temperature above 100.4°F (38°C) after injection is a red flag
One patient in South Africa developed a deep skin infection after injecting in the same spot for three weeks. She didn’t realize the redness was growing until it turned into an abscess. She needed surgery.
Why your anxiety is the hidden risk
You’re not just learning a technique. You’re learning to fight fear.
Studies show 57% of people who quit biologic therapy early did so because of anxiety - not side effects, not cost, not inconvenience. Just fear.
That fear leads to:
- Shaky hands - needle goes in crooked
- Rushed injections - device clicks but doesn’t fully activate
- Skipping steps - “I’ll just do it fast”
- Avoiding injections altogether - leading to disease flare-ups
There’s a fix: ritual.
Successful patients don’t just inject. They have a routine. Same time. Same place. Same sequence. Maybe they play a song. Maybe they light a candle. Maybe they breathe in for five counts, hold, then inject.
One study found patients who built a ritual had 53% fewer technique errors and 41% better adherence. It’s not magic. It’s psychology. Your brain learns: “This is safe. This is controlled.”
Find your ritual. Write it down. Stick to it.

What to do if your training was rushed or skipped
If you were given a pen and told to figure it out - you’re not alone. But you’re not stuck.
Here’s what to do now:
- Call your pharmacy. Ask if they have a medication therapy management (MTM) session. Many offer free injection coaching
- Search for your drug’s official website. Companies like Adbry and Humira have free video libraries with step-by-step demos
- Use a training device. Many manufacturers send them for free. If you didn’t get one, ask
- Practice on an orange. It’s the same size as skin. Practice the pinch, the click, the hold
- Record yourself. Use your phone. Watch it. Do you hold the pen right? Do you wait after clicking?
Don’t wait for your next doctor visit. Start now. One wrong injection can cost you weeks of pain - or worse.
Follow-up isn’t optional - it’s essential
One training session isn’t enough. Not even close.
Patients who had just one session had a 52% chance of using the correct technique six months later. Those who had three or more supervised practices? 94%.
Ask for:
- A follow-up call within 7 days
- A video check-in with a nurse
- A return visit to the clinic for a live demonstration
If your provider says they don’t have time - ask them to refer you to someone who does. A nurse practitioner, a pharmacist, a patient support coordinator. They exist. You just have to ask.
And if you’re still unsure after a week? Don’t guess. Call your doctor. Send a photo of the injection site. Ask: “Is this normal?”
There’s no shame in asking. There’s only risk in staying silent.
What the future holds - and how to stay ahead
The biologic market is growing fast. More people will be injecting at home. More companies are building digital tools - apps that remind you to inject, track your site rotation, and even video-call you to check your technique.
But technology won’t fix bad training. Only better systems will.
Until then, you’re your own best defense. Know the steps. Practice them. Build your ritual. Watch for signs of infection. Don’t trust a 30-minute demo. Demand more. Your health depends on it.


Daisy L
November 21, 2025 AT 21:29Anne Nylander
November 23, 2025 AT 03:19Franck Emma
November 24, 2025 AT 15:34Noah Fitzsimmons
November 25, 2025 AT 22:45Eliza Oakes
November 26, 2025 AT 12:41Logan Romine
November 26, 2025 AT 13:16Leo Tamisch
November 26, 2025 AT 20:44Corra Hathaway
November 27, 2025 AT 19:15Shawn Sakura
November 29, 2025 AT 03:46Paula Jane Butterfield
November 30, 2025 AT 07:28Simone Wood
November 30, 2025 AT 13:40Florian Moser
November 30, 2025 AT 17:36jim cerqua
December 2, 2025 AT 08:26