Drug Risk Context Calculator
This tool helps you understand how your personal factors impact the risks described in FDA black box warnings. Remember: a black box warning doesn't mean a drug is unsafe—it means you need to understand your specific risk.
What Is a Black Box Warning?
A black box warning is the strongest safety alert the U.S. Food and Drug Administration (FDA) can put on a prescription drug. It’s called that because it appears in a thick black border on the drug’s package insert - like a warning sign you can’t miss. This isn’t just a small note tucked at the bottom of a label. It’s front and center, meant to grab the attention of doctors and patients alike.
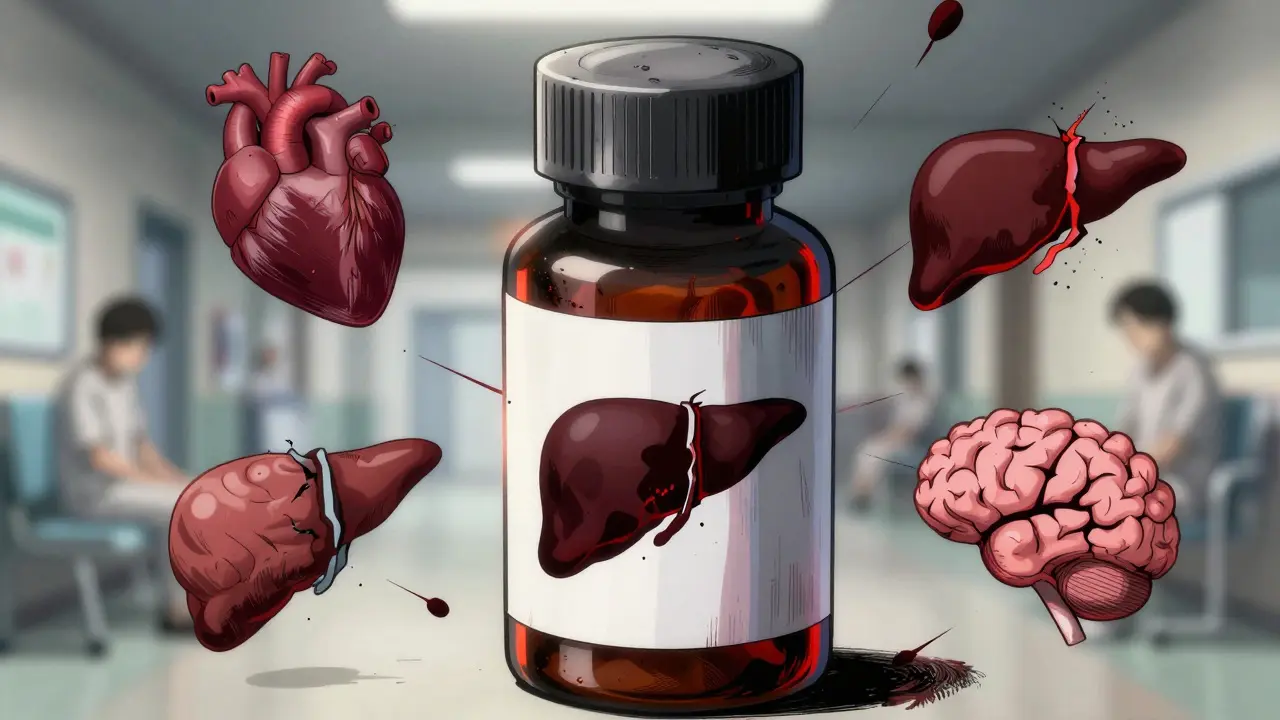
These warnings aren’t given out lightly. They’re only added when there’s solid evidence that a drug can cause serious injury or death. Think: organ failure, suicidal thoughts, life-threatening allergic reactions, or sudden heart problems. The FDA doesn’t slap these on just because something might go wrong. It’s when the risk is real, measurable, and serious enough that it could change whether a drug should be used at all.
Why Do These Warnings Exist?
The FDA introduced the black box warning system in the 1970s, but the rules were formalized after the Kefauver-Harris Amendments of 1962. That law forced drug makers to prove their products were not just safe, but actually effective. Over time, the black box became the tool to flag the most dangerous side effects.
Today, more than 400 medications carry this warning. That includes drugs for diabetes, depression, epilepsy, chronic pain, and even some antibiotics. The goal isn’t to scare people away from medicine - it’s to make sure no one takes a drug without fully understanding the stakes.
For example, some antidepressants carry black box warnings because they can increase suicidal thoughts in young adults under 25. That doesn’t mean you shouldn’t take them. It means your doctor needs to monitor you closely, especially in the first few weeks. The warning exists so no one misses that detail.
How Are These Warnings Decided?
The FDA doesn’t wake up one day and decide to add a black box warning. It’s a long, careful process.
First, a drug goes through lab tests, animal studies, and clinical trials with hundreds or thousands of people. Even then, rare side effects might not show up until the drug is used by millions. That’s why the FDA keeps watching after approval - through the FDA Adverse Event Reporting System (FAERS). Doctors, patients, and pharmacies can report problems. When enough reports point to the same serious issue, the FDA investigates.
If the evidence is strong enough, the agency will require the drug maker to add a black box warning. Sometimes, this happens years after the drug hits the market. Take rosiglitazone, a diabetes drug. After reports of heart attacks piled up, the FDA added the warning in 2007. Usage dropped by 70%. But not all drugs see that kind of reaction. Pioglitazone, a similar drug with the same warning, didn’t see the same drop - partly because it got less media attention.
What Does a Black Box Warning Actually Say?
These aren’t vague statements. They’re specific. A black box warning might say:
- “May cause severe liver damage - monitor liver enzymes monthly.”
- “Contraindicated in patients with a history of heart failure.”
- “Risk of suicidal behavior in children and adolescents - increase monitoring during initial treatment.”
- “Do not use with alcohol or other CNS depressants.”
Some warnings even require special training before a doctor can prescribe the drug. Others limit use to certain patients - like those who’ve tried other treatments first. The goal is to make sure the drug is only used when the benefit clearly outweighs the risk.
Are Drugs With Black Box Warnings Always Dangerous?
No. And that’s a common misunderstanding.
A black box warning doesn’t mean “don’t take this.” It means “this is powerful, and you need to know exactly what you’re getting into.”
Take methotrexate, used for rheumatoid arthritis and some cancers. It can cause liver damage and bone marrow suppression - serious stuff. But for someone with severe arthritis who hasn’t responded to other drugs, methotrexate can be life-changing. The warning ensures the doctor checks blood counts and liver function regularly. That’s not a dealbreaker - it’s a safety net.
As pharmacists at the Cleveland Clinic explain, the conversation matters more than the warning. If your doctor says, “This drug has a black box warning, but here’s why I think it’s right for you, and here’s how we’ll keep you safe,” that’s a good sign. It means they’re thinking carefully.
How Do These Warnings Affect Prescribing?
Studies show black box warnings change behavior - but not always the way you’d expect.
When the FDA added a warning about rosiglitazone’s heart risks, prescriptions dropped sharply. But for other drugs, the effect was minimal. Why? Because doctors don’t just react to warnings - they react to their patients’ needs. If a patient has no other options, the warning might not stop a prescription. It just makes the doctor more cautious.
Some doctors use tools like the Drug Effectiveness Review Project or Consumer Reports Best Buy Drugs to compare options. These sites help them weigh risks, costs, and effectiveness - not just look at the warning.
And patients? They should ask questions. If your prescription comes with a black box warning, ask: What’s the exact risk? How often does it happen? Are there safer alternatives? What tests or check-ups will I need?
What Should You Do If Your Medication Has a Black Box Warning?
Don’t panic. Don’t stop taking it without talking to your doctor. But do take action.
- Read the warning. It’s in the patient information leaflet that comes with your prescription.
- Ask your doctor: What are the signs of the serious side effect? When should I call for help?
- Find out if you need blood tests, heart scans, or other monitoring - and stick to the schedule.
- Tell your doctor about every other drug, supplement, or herb you’re taking. Some interactions can turn a low risk into a high one.
- Report any strange symptoms to the FDA through MedWatch. Your report could help protect others.
Also, don’t assume a drug without a black box warning is automatically safer. Many dangerous drugs don’t have them - not because they’re safe, but because the evidence hasn’t been gathered yet.
Are These Warnings Working?
They’re not perfect. Some patients never see the warning. Some doctors skip reading the full label. And media coverage plays a huge role - a warning that makes the news gets more attention than one that doesn’t.
But the system works when it’s used right. The FDA continues to update warnings as new data comes in. In recent years, black box warnings have been added to opioids, certain psychiatric drugs, and even some weight-loss medications after reports of strokes and heart attacks.
Experts are pushing for better formats - ones that show absolute risk (“1 in 100 people may have this side effect”) instead of vague language like “risk of serious injury.” That helps patients understand what the numbers really mean.
Final Thoughts
Black box warnings are the FDA’s loudest alarm. They’re not meant to scare you away from medicine - they’re meant to make sure you and your doctor make the best possible choice. The right drug, used the right way, can save your life. The wrong one, taken without understanding the risks, can end it.
If you’re on a medication with a black box warning, you’re not being treated as a risk. You’re being treated as someone who deserves to know the truth - and who deserves to be protected by it.

Sheila Garfield
January 29, 2026 AT 12:52Shawn Peck
January 29, 2026 AT 23:30Jason Xin
January 30, 2026 AT 03:11Donna Fleetwood
January 30, 2026 AT 16:34Melissa Cogswell
January 31, 2026 AT 19:18Diana Dougan
February 1, 2026 AT 20:22Bobbi Van Riet
February 2, 2026 AT 21:38Holly Robin
February 4, 2026 AT 11:05Shubham Dixit
February 5, 2026 AT 16:07KATHRYN JOHNSON
February 7, 2026 AT 06:37Blair Kelly
February 7, 2026 AT 07:21