Every year, over 900,000 people in the U.S. have a stroke caused by a blood clot. For many, that clot forms because of a heart rhythm problem called atrial fibrillation - or Afib. When the heart beats irregularly, blood can pool and clot in the upper chambers. If that clot travels to the brain, it causes an ischemic stroke. The good news? Blood thinners - or anticoagulants - can cut that risk by two-thirds. The challenge? Choosing the right one.
What Are Blood Thinners Really Doing?
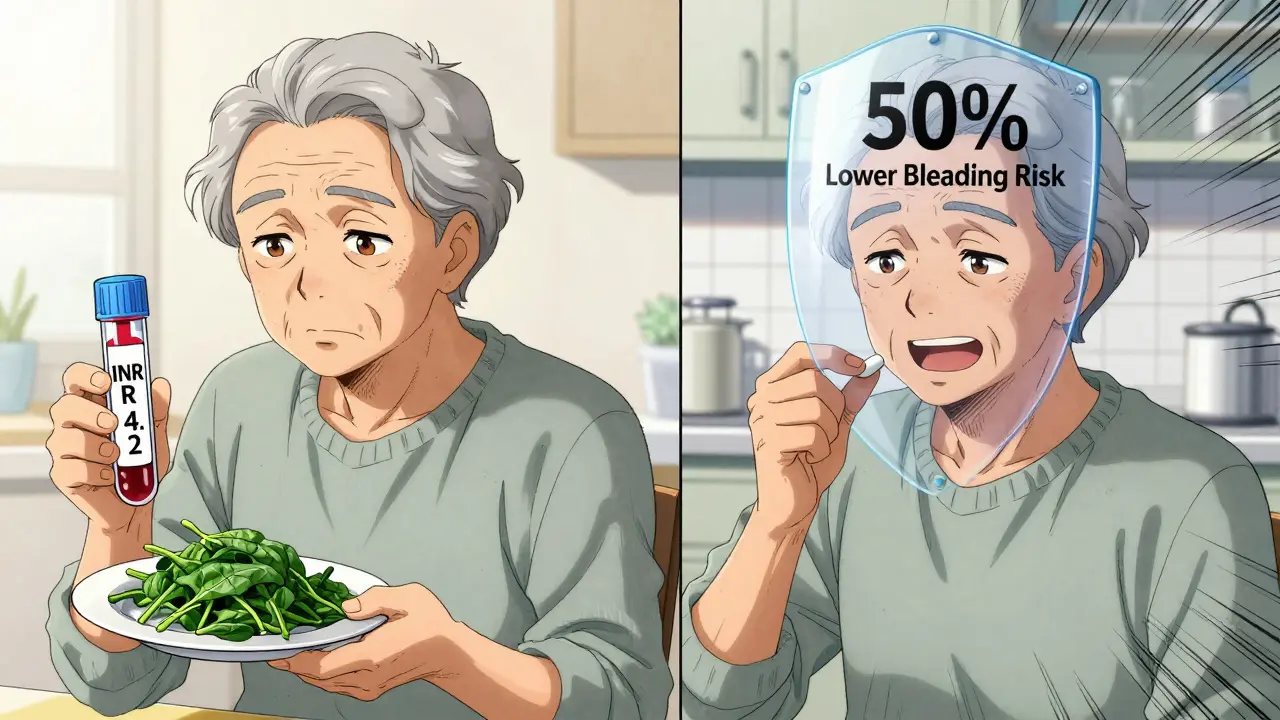
They don’t actually thin your blood. That’s a myth. Instead, they slow down the clotting process by targeting specific proteins in your blood. There are two main types: warfarin and the newer group called DOACs (direct oral anticoagulants), also known as NOACs.Warfarin has been around since the 1950s. It works by blocking vitamin K, which your liver needs to make clotting factors. But here’s the catch: vitamin K is in leafy greens like spinach, kale, and broccoli. So if you eat more greens one week and less the next, your blood clotting time changes. That’s why people on warfarin need regular blood tests - called INR checks - to make sure their dose is just right. The target range is 2.0 to 3.0. If it’s too low, you’re at risk for stroke. Too high, and you might bleed internally.
DOACs - like apixaban, rivaroxaban, dabigatran, and edoxaban - work differently. They lock onto specific clotting factors directly. Apixaban and rivaroxaban block factor Xa. Dabigatran blocks thrombin (factor IIa). Because they’re more targeted, they don’t need constant blood tests. You take the same dose every day, no matter what you eat. And they work faster. Where warfarin takes 5 to 7 days to reach full effect, DOACs kick in within hours.
Which One Works Better?
Large studies involving over 2 million patients show DOACs are safer and just as effective as warfarin - and often better. A 2021 review found DOACs reduced stroke risk by 23% and major bleeding by 32% compared to warfarin. The biggest win? Intracranial bleeding (bleeding in the brain). DOACs cut that risk by more than half. That’s huge. A brain bleed is often deadly or disabling. Warfarin carries a much higher risk.Among DOACs, apixaban stands out. In head-to-head trials, it had the lowest rate of major bleeding. It’s also the most prescribed DOAC in the U.S., with nearly half of new prescriptions going to it. Why? It’s forgiving. If you’re older, lighter, or have mild kidney issues, your dose can be lowered without losing protection. Rivaroxaban is taken once a day, which some people like. Dabigatran works well but has a higher chance of stomach upset - about 1 in 3 users report nausea or bloating. Edoxaban is less commonly used but still effective.
Warfarin isn’t obsolete. It’s still the go-to for people with mechanical heart valves. DOACs have been shown to increase clot risk in those patients. It’s also preferred for severe mitral stenosis. And if you’re on dialysis or have very poor kidney function, warfarin might still be your best option - though even that’s debated. For most people with Afib and no mechanical valves? DOACs are the clear first choice.
Cost Matters - But Not Like You Think
Warfarin costs about $10 a month for the pill. Sounds cheap, right? But add in the cost of 12 to 16 INR tests a year - $15 to $25 each - and you’re spending $300 to $400 annually just on monitoring. Plus, if you go off track, you might end up in the ER. That’s not factored into the sticker price.DOACs used to cost $600 to $700 a month. That’s a barrier for many. But as of early 2024, all major DOACs have generic versions available. Generic apixaban now runs $450 to $500. Rivaroxaban and dabigatran are even lower - around $550 and $500, respectively. Edoxaban is still brand-only, so it’s pricier. For Medicare beneficiaries, copays are often under $20 with generic DOACs. That’s less than the cost of a single INR test.
One patient on Reddit put it simply: “I switched from warfarin to apixaban after 10 years. No more worrying about broccoli. No monthly blood draws. My neurologist says my bleeding risk is 50% lower.” That’s not just convenience - it’s peace of mind.
Who Should Avoid DOACs?
DOACs aren’t for everyone. If you have a mechanical mitral valve, DOACs are dangerous. The RE-ALIGN trial showed dabigatran tripled the risk of clots in those patients. Avoid them.Extreme body weight matters too. If you weigh less than 60 kg (132 lbs) or more than 120 kg (265 lbs), DOACs may not be dosed correctly. There’s limited data in these groups. Warfarin, with its INR monitoring, gives doctors more control.
Severe kidney disease - CrCl under 15 mL/min - is another red flag. DOACs are cleared by the kidneys. In advanced kidney failure, they can build up and increase bleeding risk. Warfarin is safer here, though still risky.
And if you’re on multiple medications that interact with DOACs - like certain antifungals, HIV drugs, or seizure meds - warfarin might be easier to manage. You can adjust the dose based on INR. With DOACs, you’re stuck with fixed doses. No easy tweaks.
Monitoring and Safety
You don’t need blood tests with DOACs - but you still need to check in. Kidney function should be tested every 6 to 12 months. If you’re over 75 or have diabetes, every 6 months is better. If your kidneys start to fail, your doctor may lower your dose or switch you.Everyone on anticoagulants needs to know the signs of bleeding: unusual bruising, blood in urine or stool, severe headaches, vomiting blood, or sudden weakness. Don’t wait. Go to the ER.
There are reversal agents now. If you bleed badly on dabigatran, idarucizumab can undo it in minutes. For apixaban or rivaroxaban, andexanet alfa works. Warfarin can be reversed with vitamin K and fresh plasma, but it takes hours. The fact that reversal drugs exist makes DOACs safer than ever.
Real-World Experience
Patients on DOACs report higher satisfaction. A 2023 survey of over 12,000 users found 78% preferred DOACs over warfarin. Why? No dietary restrictions. No monthly blood draws. Fewer hospital visits. Warfarin users, on the other hand, complain about the constant monitoring and the stress of keeping vitamin K levels stable. One man said, “I used to plan my meals around my INR. I stopped eating salads for years.”But DOACs aren’t perfect. Some users report stomach upset, especially with dabigatran. Others worry about the cost - even with generics. And if you miss a dose, you’re unprotected faster than with warfarin. Apixaban has a half-life of about 12 hours. Skip a dose, and your protection drops quickly. That’s why adherence is critical.
What’s Next?
The future of anticoagulants is coming. New drugs like milvexian and abelacimab are in late-stage trials. They target different parts of the clotting system and may cut bleeding risk even further - without losing stroke protection. One early study showed abelacimab reduced major bleeding by nearly half compared to apixaban.Soon, genetic testing may guide your choice. Some people metabolize warfarin slowly because of a gene variant (CYP2C9). Others absorb DOACs poorly due to another (ABCB1). In the next five years, a simple blood test could tell your doctor which drug is right for you - not just based on age or kidney function, but your biology.
For now, the message is clear: If you have nonvalvular atrial fibrillation and are at risk for stroke, DOACs are the best option for most people. They’re safer, easier, and now affordable. Talk to your doctor about your risk score - CHA₂DS₂-VASc - and your bleeding risk - HAS-BLED. Don’t assume warfarin is the default. Ask about apixaban. Ask about the generics. Your brain will thank you.


Edith Brederode
January 19, 2026 AT 19:22Thank you for this incredibly clear breakdown! 🙌 I switched to apixaban last year after a scary INR spike, and honestly? Life feels lighter. No more counting spinach. No more Friday morning clinic trips. I actually forgot I was on blood thinners until I saw my pill organizer the other day. Peace of mind is worth more than any pill price tag.
Art Gar
January 20, 2026 AT 15:33While the data appears favorable, one must consider the broader pharmaceutical ecosystem. The promotion of DOACs coincides with a systematic dismantling of traditional anticoagulation clinics, which historically provided not only monitoring but also patient education and nutritional counseling. The convenience narrative masks a corporate-driven erosion of holistic care. One wonders whether the reduction in INR tests is truly a benefit-or merely a cost-cutting measure disguised as innovation.
clifford hoang
January 22, 2026 AT 13:31Let’s be real-DOACs are just a Trojan horse. The FDA approved them because Big Pharma needed a new cash cow after warfarin’s patent expired. Ever notice how every single ad for apixaban shows a happy couple hiking? Meanwhile, the real data? Buried in paywalled journals. And don’t get me started on the reversal agents-those are ridiculously expensive, and hospitals stock them only because they’re legally required. It’s all a scam. The government knows warfarin is safer. They just don’t want to admit it because the DOACs are too profitable. 🤫👁️🗨️
Emily Leigh
January 23, 2026 AT 13:51Ugh, I hate when people act like DOACs are magic. I took rivaroxaban for 8 months and got a GI bleed that landed me in the ER. They said it was "rare," but it happened to ME. And now I’m stuck on warfarin again because my kidney function dropped. So much for "safer." Also, who even has time to get kidney tests every 6 months? I work two jobs. 😩
Renee Stringer
January 24, 2026 AT 00:27It is concerning that the emphasis on convenience overshadows the importance of individualized care. While DOACs offer statistical advantages, they are not universally appropriate. The assumption that all patients with nonvalvular AFib are candidates for DOACs reflects a troubling trend toward protocol-driven medicine, where nuance is sacrificed for efficiency. This is not medicine-it is management.
Crystal August
January 24, 2026 AT 19:31So let me get this straight-you’re telling me I can just take a pill and never think about it again? No more blood tests? No more worrying about broccoli? That’s great for people who don’t have to worry about their kidneys, their meds interacting with their 17 other prescriptions, or their insurance denying coverage because they "don’t qualify." Meanwhile, I’m still on warfarin because my doctor says I’m "too complex." Thanks, healthcare system. 🙃
Nadia Watson
January 26, 2026 AT 08:59Thank you for sharing this. I’ve been on apixaban for 3 years now, and I’m so grateful for the stability. I’m a retired nurse, so I know how easy it is to overlook the small things-like kidney function. I get mine checked every 6 months, and I remind my friends to do the same. One thing I wish more people knew? It’s not just about the drug-it’s about staying connected to your care team. Even if you don’t need blood tests, you still need to talk to someone who understands your whole picture. 🌿
Courtney Carra
January 26, 2026 AT 18:09There’s a quiet tragedy here: we’ve turned anticoagulation into a consumer product. We market it like a smartphone upgrade-"New and Improved!" But the body isn’t an app. You can’t just download a new version and expect everything to work. Some of us are still living with the consequences of rushed approvals, hidden risks, and the erosion of clinical judgment. I’m not anti-DOAC-I’m pro-compassionate science.
thomas wall
January 28, 2026 AT 13:12The notion that DOACs are "better" is statistically misleading. The reduction in intracranial hemorrhage is indeed significant-but this benefit is concentrated in a subset of the population. For elderly patients with multiple comorbidities, the overall mortality benefit remains ambiguous. Furthermore, the absence of routine monitoring removes a crucial safety net: the opportunity for early detection of renal decline, drug interactions, or non-adherence. One must ask: are we optimizing outcomes-or merely reducing healthcare burden?
Shane McGriff
January 28, 2026 AT 17:04Emily, I hear you. I’ve been there-GI bleed, kidney issues, insurance denials. It’s not fair. But here’s what I’ve learned: your doctor isn’t trying to make your life harder. They’re trying to balance risk, and sometimes that means warfarin is still the right call. Don’t give up. Ask for a referral to a hematologist. Get a second opinion. And if your meds are too expensive, ask about patient assistance programs-most pharma companies have them. You’re not alone in this. And your voice matters. Keep pushing.