More people are using CBD for sleep, pain, or anxiety-but few realize how deeply it can interfere with their prescription meds. If you're on blood thinners, heart meds, thyroid medicine, or seizure drugs, mixing CBD could put you in serious danger. This isn't speculation. It's backed by clinical reports, FDA warnings, and real patient outcomes.
How CBD Changes How Your Meds Work
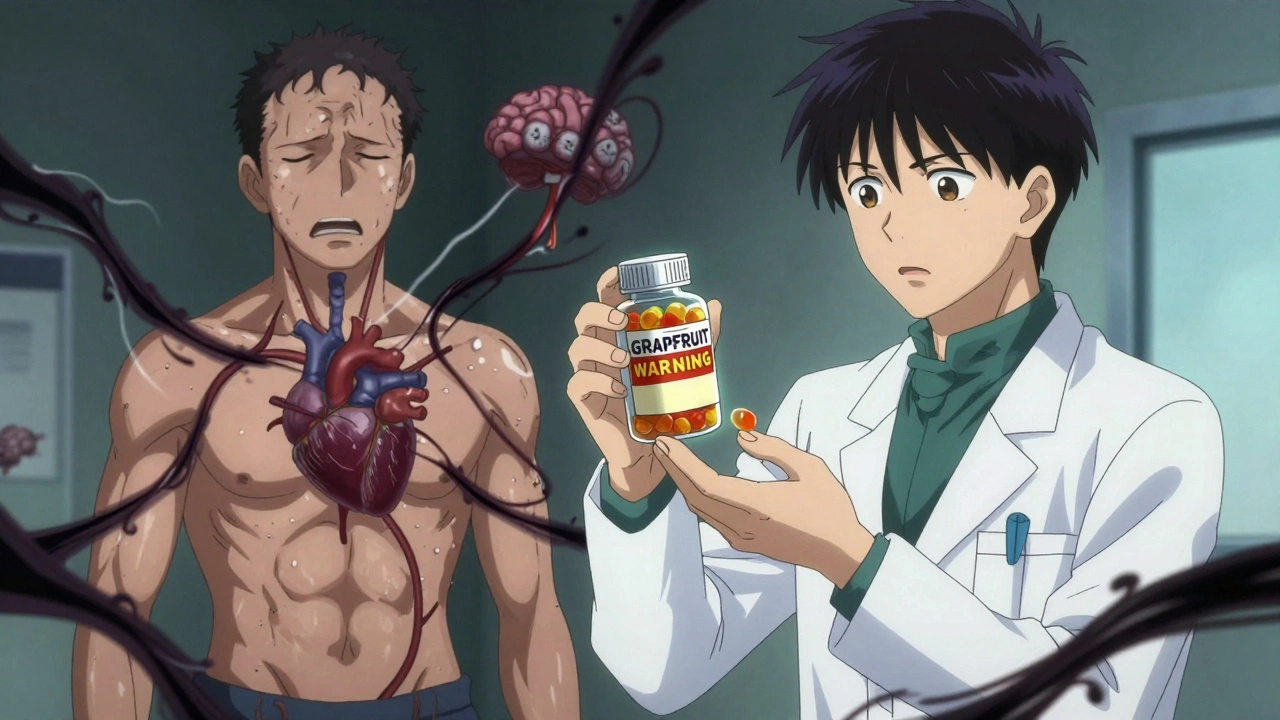
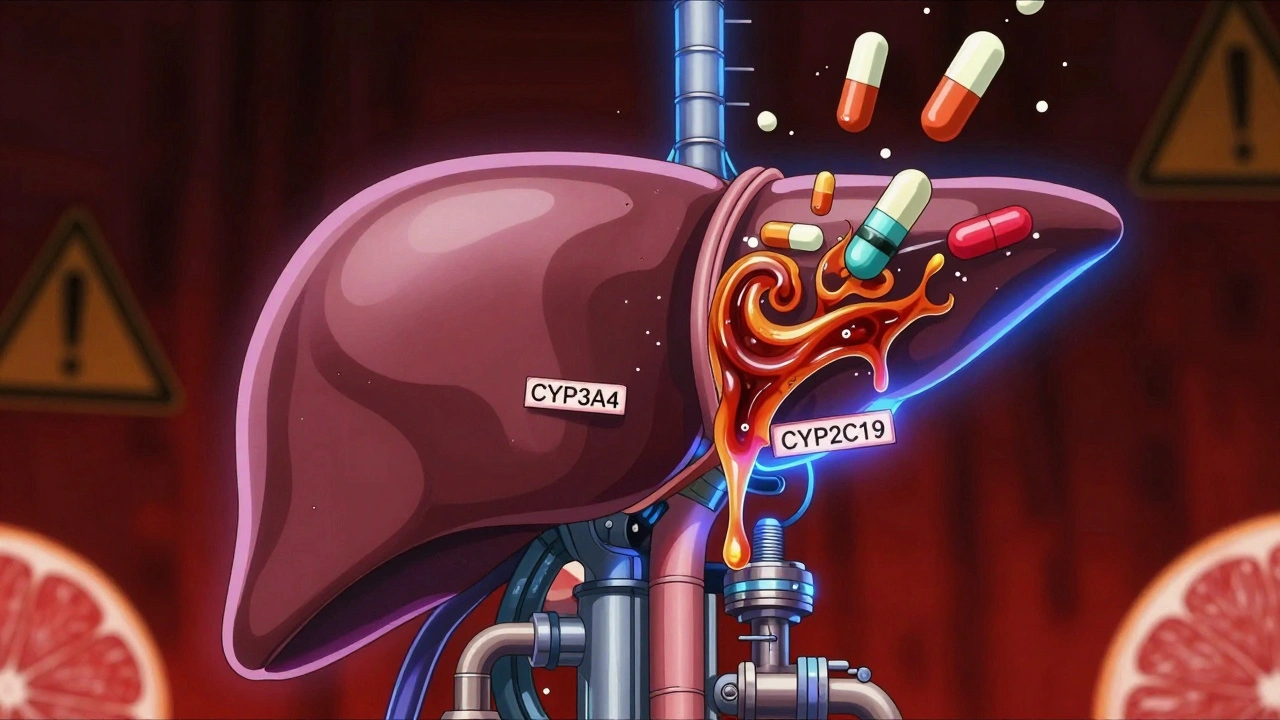
CBD doesn't just float through your body unnoticed. It hits your liver hard-specifically, the cytochrome P450 enzyme system. This system is responsible for breaking down about 95% of all prescription drugs. When CBD enters the picture, it acts like a clog in the pipeline. It slows down or even blocks the enzymes that normally process your medications.
That means your drugs don't get broken down the way they should. Instead, they build up in your bloodstream. For some meds, even a small increase can be dangerous. Think of it like turning up the volume on a song you're already listening to-too loud, and it distorts. Too much of your medicine in your blood? That's when side effects turn into emergencies.
The two main enzymes CBD messes with are CYP3A4 and CYP2C19. These are the same ones that handle drugs like warfarin, amiodarone, levothyroxine, and clobazam. If you're taking any of these, CBD isn't just a harmless supplement. It's a potential trigger for overdose.
Medications That Can Turn Dangerous With CBD
Not all drugs are equally risky. But some are so sensitive that even a tiny change in blood levels can cause harm. These are called Narrow Therapeutic Index (NTI) medications. They have a very small window between being effective and being toxic.
- Warfarin: A blood thinner. CBD can cause levels to spike, leading to uncontrolled bleeding. Seven documented cases required dose changes; two patients had serious bleeding events.
- Amiodarone: Used for irregular heartbeats. CBD can push levels into the toxic range, increasing risk of lung or liver damage.
- Levothyroxine: For hypothyroidism. CBD may reduce its absorption, making you feel fatigued, cold, or gain weight-even if you're taking your pill on time.
- Clobazam, Valproate, Lamotrigine: Anti-seizure drugs. CBD can increase their levels by 2-3 times, causing drowsiness, confusion, or even coma in extreme cases.
- Tacrolimus and Sirolimus: Immunosuppressants after organ transplants. CBD can cause toxic buildup, raising infection risk and organ rejection chances.
Here's the kicker: if your pill bottle says "Avoid grapefruit", you should also avoid CBD. Both grapefruit and CBD block the same liver enzyme (CYP3A4). That’s not a coincidence-it’s a red flag.
Why CBD Is Riskier Than Other Cannabinoids
Not all cannabis compounds are the same. CBD is a powerful inhibitor of CYP3A4-much stronger than CBG or CBN. That means even if you're not using THC, CBD alone is enough to cause problems.
Studies show that CBD's effects can last for days after you stop taking it. That's because it builds up in your system over time, especially with daily use. So even if you take your pill in the morning and CBD at night, the enzyme blockage doesn't just disappear overnight. The interference lingers.
One 2023 review found 31 documented cases of dangerous interactions across 889 patients using cannabinoids. Most involved NTI drugs. And these are just the cases that were reported. Many more likely went unnoticed.
What Happens to Your Liver?
CBD isn't just messing with your meds-it can hurt your liver directly. In clinical trials for Epidiolex (a prescription CBD product), about 20% of patients saw elevated liver enzymes. That's a sign your liver is under stress.
If you already have liver disease, fatty liver, or drink alcohol regularly, CBD could make things worse. The FDA's prescribing info for Epidiolex says it's contraindicated in people with moderate to severe liver impairment. That's not a suggestion-it's a hard rule.
And it's not just about the dose. A 2022 SAMHSA report listed liver toxicity as one of the top three risks of CBD use. That’s why doctors recommend blood tests before and after starting CBD if you're on meds that affect the liver.
When CBD Makes You Sleepy-And Why That’s Dangerous
CBD can make you drowsy. So can opioids, benzodiazepines like Xanax or Ativan, sleep aids, antihistamines like Benadryl, and even alcohol.
Put them all together? You're not just tired-you're at risk for falls, car accidents, or even respiratory depression. One study documented cases where patients on CBD and sedatives had trouble waking up after surgery. Anesthesiologists had to adjust dosages because CBD was still in their system days after last use.
If you're taking any of these drugs, don't assume CBD is "safe" just because it's "natural." The combination doesn't cancel out risk-it multiplies it.
What You Should Do Right Now
If you're on any prescription medication and thinking about trying CBD-or already using it-here's what to do:
- Check your pill bottles. Look for the grapefruit warning. If it's there, CBD is likely unsafe with that drug.
- Make a full list of everything you take. Include prescriptions, OTC meds, supplements, and herbal products. Don’t forget vitamins, melatonin, or St. John’s Wort.
- Talk to your pharmacist. They’re trained to spot drug interactions. Bring your CBD product with you-even if it’s labeled "hemp oil" or "CBD isolate." They can check the exact concentration and ingredients.
- Don’t start CBD without telling your doctor. Especially if you're on heart, thyroid, seizure, or immune drugs.
- If you already use CBD, get blood tests. For drugs like warfarin, tacrolimus, or levothyroxine, your doctor can check your levels before and after starting CBD to see if adjustments are needed.
- Start low and go slow-if you proceed at all. If your doctor says it’s okay, begin with 5-10mg of CBD and wait at least 4-6 hours before taking your prescription. Never combine them at the same time.
What About Low-Dose CBD?
Some people say low doses of CBD are safe. Dr. Ethan Russo has suggested the risk is overstated for small amounts. But here’s the problem: there’s no proven safe threshold. A 10mg dose of CBD might be fine for one person and dangerous for another, depending on their liver enzymes, genetics, or other meds.
And what counts as "low dose"? There’s no standard. A gummy might say 10mg, but testing shows many products contain 20-30% more than labeled. A 2023 analysis found that only 68% of top CBD brands provide third-party lab results. That means you don’t even know what you’re really taking.
Until we have better regulation and testing, assuming "low dose = safe" is gambling with your health.
What’s Being Done About It?
The FDA has received over 4,800 reports of CBD-related adverse events through September 2023. Not all are about drug interactions-but enough are to warrant concern.
In February 2024, the FDA announced new rules: by Q3 2024, all CBD products sold in the U.S. must include clear warnings about potential drug interactions on their labels. That’s a big step. But until then, you can’t rely on packaging. You have to ask questions.
Researchers at Penn State also built a free online tool called CANN-DIR that helps patients and doctors check for possible interactions between CBD and prescription drugs. It’s not perfect-but it’s better than guessing.
Bottom Line: Don’t Guess. Test. Ask.
CBD isn’t the villain. But treating it like a harmless herb is dangerous. It’s a powerful biological agent that changes how your body handles medicine. For millions of people, that change could mean hospitalization-or worse.
If you're on any prescription drug, especially heart, thyroid, seizure, or blood-thinning meds, don't add CBD without professional guidance. Your pharmacist is your best first stop. Your doctor is your second. And your liver? It doesn’t get a second chance.
Can I take CBD with my blood thinner like warfarin?
No-unless your doctor closely monitors your INR levels. CBD can cause warfarin to build up in your blood, increasing bleeding risk. Seven documented cases required dose adjustments, and two patients had serious bleeding. Do not combine them without medical supervision.
Does CBD interact with antidepressants or anxiety meds?
Yes. CBD can increase levels of some antidepressants and benzodiazepines like Xanax or Ativan. This raises the risk of excessive drowsiness, dizziness, and impaired coordination. In rare cases, it can lead to respiratory depression, especially if combined with alcohol or opioids.
Is CBD safe if I don’t take any medications?
For healthy people not on meds, low-dose CBD is generally well-tolerated. But it can still cause liver enzyme changes in about 20% of users, especially at higher doses. If you have any liver condition, even without meds, CBD may not be safe.
What should I do if I’ve already been taking CBD with my meds?
Stop CBD immediately and contact your doctor or pharmacist. Ask for a blood test to check levels of your medications-especially if you’re on warfarin, thyroid meds, or seizure drugs. Don’t wait for symptoms. Some interactions cause damage before you feel anything.
Are there CBD products that don’t interact with meds?
No. All CBD products-whether isolate, broad-spectrum, or full-spectrum-interact with the same liver enzymes. The only difference is potency. Even "low-dose" products can be risky if you’re on sensitive medications. Avoid CBD entirely if you’re on a narrow therapeutic index drug.
Can I use CBD if I’ve had a transplant?
No. CBD has been shown to dangerously increase levels of immunosuppressants like tacrolimus and sirolimus. This raises the risk of organ rejection and life-threatening infections. The Portland Clinic and other transplant centers advise patients to avoid CBD completely.
Why do some people say CBD is safe with meds?
Some researchers suggest low doses may be safe, but clinical evidence is lacking. Most reports of "safe" use are anecdotal. Real-world data shows clear, documented cases of toxicity and hospitalizations. When lives are at risk, anecdote isn’t enough. Always rely on medical guidance, not online testimonials.

Aidan Stacey
December 12, 2025 AT 05:58CBD isn't some magic herb your cousin swears by on Instagram. It's a potent liver enzyme blocker, and if you're on warfarin or thyroid meds, you're playing Russian roulette with your health. I've seen patients bleed out because they thought 'natural' meant 'safe.' It doesn't. Stop self-diagnosing with TikTok advice and talk to your pharmacist.
And yes, if your pill says 'avoid grapefruit,' CBD is right there with it. Same enzyme. Same danger. Same hospital trip.
Stop romanticizing cannabinoids. This isn't yoga. This is pharmacology.
And if you're one of those people saying 'I take 5mg, it's fine' - you're not a pioneer. You're a statistic waiting to happen.
Jean Claude de La Ronde
December 13, 2025 AT 09:02so like… if i take cbd and my blood thinner… is that like… putting a banana in my car’s gas tank? bc that’s what it sounds like. also why is everyone acting like this is new info? my grandma knew grapefruit and meds don’t mix in the 80s. why is cbd suddenly the boogeyman? also who made this article? a pharmacist who hates fun?
Mia Kingsley
December 14, 2025 AT 12:17OMG I’ve been taking CBD with my levothyroxine for 8 months and I feel AMAZING. My energy’s up, my skin’s glowing, and I sleep like a baby. Your article is so fear-mongering. I’m not some lab rat. I’m a human being who listens to her body. Also, the FDA? Please. They banned ephedrine and now we have fentanyl crises. Who’s really in charge here?
And FYI, my CBD gummy says ‘10mg’ but I swear it’s more like 25. That’s why it works. You’re all just scared of natural healing. Wake up.
Also, I don’t trust pharmacists. They’re just drug pushers in lab coats.
Also also - I took CBD with Xanax and didn’t die. So your ‘dangerous’ is my ‘perfect combo.’
Katherine Liu-Bevan
December 16, 2025 AT 01:31Let’s be clear: this isn’t about demonizing CBD. It’s about understanding pharmacokinetics. The CYP3A4 and CYP2C19 enzymes don’t care if you call it ‘hemp oil’ or ‘wellness tonic.’ They process drugs the same way. If you’re on a narrow therapeutic index medication - warfarin, tacrolimus, levothyroxine - the margin for error is millimeters, not miles.
There are documented cases of INR spikes from CBD use. There are documented cases of transplant rejection. There are documented cases of respiratory depression when combined with benzodiazepines.
This isn’t opinion. It’s clinical data. And if you’re reading this and you’re on any of these meds - stop self-experimenting. Talk to your provider. Get a blood test. Your liver doesn’t have a ‘maybe’ setting.
And yes - if your pill says ‘avoid grapefruit,’ CBD belongs in that same warning box. No exceptions.
Aman deep
December 16, 2025 AT 10:23Bro, I live in Delhi and I’ve been taking CBD oil with my blood pressure meds for 11 months. No issues. My uncle in Punjab uses it with his diabetes pills too. Maybe it’s not the same for everyone? I think the real problem is that Western medicine doesn’t understand plant medicine. We’ve been using herbs for thousands of years - why are we suddenly scared?
Also, I don’t trust big pharma. They make the meds, then they scare us about the natural stuff. It’s all about control.
But hey - if you’re worried, get your levels checked. That’s smart. But don’t throw the whole plant out because one person got unlucky.
Also, my CBD oil is from a local farmer. No labels. No third-party tests. But it’s pure. You can taste the earth in it. That’s more real than any lab report.
Sylvia Frenzel
December 18, 2025 AT 05:54So now we’re banning natural remedies because some corporate lab in New Jersey says so? What’s next? Banning sunlight because it can cause skin cancer? CBD is not a drug. It’s a plant. And if you’re too weak to handle a little herb while on your pills, maybe you shouldn’t be on pills at all.
Also, the FDA is a joke. They approved opioids for years and now they’re mad about CBD? Wake up, America. This is just another way to control the masses and keep you buying overpriced pharmaceuticals.
I’ve been taking CBD with my antidepressants for two years. I’m happier, calmer, and my doctor hasn’t fired me yet. So your ‘dangerous’ is my ‘liberation.’
Doris Lee
December 19, 2025 AT 07:03Hey everyone - I just started CBD last month for anxiety and I’m terrified now. I’m on levothyroxine. I didn’t know about the interaction. I’m going to my pharmacist tomorrow. Thank you for this post. You saved me from a mistake I didn’t even know I was making. You’re all so lucky to have access to this info. I’m grateful.
Also - if you’re on meds, please, just check with someone. It’s not weak to ask. It’s wise.
Jack Appleby
December 20, 2025 AT 10:55Let’s be candid: this article is a masterclass in overblown caution. The CYP450 system is not a fragile porcelain doll - it’s a biological workhorse. Yes, CBD inhibits it. So does St. John’s Wort. So does grapefruit. So does turmeric. So does green tea. Do we ban all of them? No. We educate.
And let’s not pretend the pharmaceutical industry is innocent here. They profit from polypharmacy. They profit from fear. They profit from patients who never question their prescriptions.
Yes, some interactions are real. But blanket warnings are the hallmark of lazy medicine. The real issue? Lack of standardized dosing and regulation - not CBD itself.
And for the love of science - stop calling it ‘hemp oil.’ It’s cannabidiol. Use the term. Think like a scientist, not a wellness influencer.
Frank Nouwens
December 21, 2025 AT 20:36Thank you for the thorough and clinically grounded overview. The distinction between anecdotal experience and pharmacological mechanism is critical here. The cytochrome P450 inhibition is well-documented, peer-reviewed, and replicated across multiple studies. The risk is not hypothetical.
I would add that even low-dose, isolate CBD products can accumulate in hepatic tissue with chronic use, leading to prolonged enzyme suppression. This is not a transient effect.
Patients must be advised to discontinue CBD at least 72 hours prior to any procedure requiring sedation, due to the lingering effects.
And yes - if your medication has a grapefruit warning, CBD should be treated with the same caution. This is not alarmism. This is standard pharmacokinetic practice.
Aileen Ferris
December 23, 2025 AT 18:01wait so if i take cbd with my anti-seizure meds and i dont have seizures anymore… is that bad? bc i feel better. like… my brain doesnt feel like mush anymore. also why is everyone acting like this is new? my neurologist told me to try it 3 years ago. you guys are late to the party.
Michelle Edwards
December 24, 2025 AT 08:52I know this sounds scary but you’re not alone. I was on warfarin and started CBD for sleep. I didn’t realize the risk until I had a weird bruise on my thigh. I went to my pharmacist - they checked my INR. It was sky-high. We stopped the CBD, adjusted my dose, and now I’m safe.
It’s not about fear. It’s about awareness. You don’t have to quit CBD forever - but you need to do it with a plan. Talk to someone who knows your meds. Your life matters more than a trend.
Sarah Clifford
December 26, 2025 AT 04:33so like… i took cbd with my xanax and i didn’t die so it’s fine. also my dog takes it and he’s chill now. why are humans so scared of plants? we’re literally the only species that overthinks everything.
Regan Mears
December 27, 2025 AT 09:16Let me be blunt: if you’re on a narrow therapeutic index drug and you’re still using CBD without medical oversight, you’re not brave - you’re reckless. This isn’t a debate. It’s a matter of physiology.
I’ve seen patients with transplants nearly lose their organs because they thought ‘natural’ meant ‘safe.’ I’ve seen people bleed internally because they didn’t get their INR checked.
And yes - if your pill says ‘avoid grapefruit,’ CBD is in that same category. Full stop.
But here’s the good news: you can still use CBD - if you’re monitored. Get blood tests. Talk to your doctor. Adjust your meds. There’s a safe path. But it requires humility. Not hype.
You don’t have to be a hero. You just have to be smart.