When you hear celiac disease, you think of bloating, diarrhea, or stomach pain. But for nearly one in three people with untreated celiac disease, the problem isn’t just in the gut-it’s in the liver. Elevated liver enzymes often show up on blood tests before digestive symptoms become obvious. And yet, most doctors don’t connect the dots. If your liver numbers are high and no one can explain why, celiac disease might be the hidden cause.
Why Your Liver Shows Up Abnormal with Celiac Disease
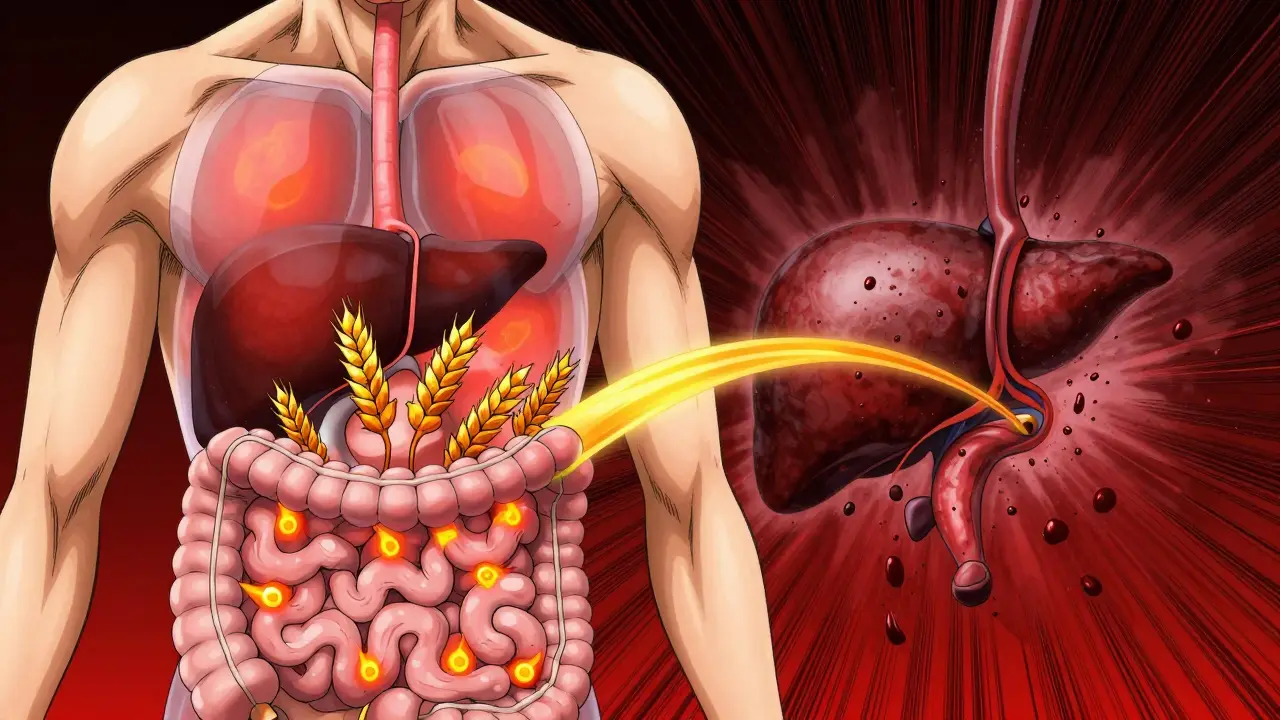
Celiac disease is an autoimmune condition triggered by gluten. When someone with celiac eats gluten, their immune system attacks the tiny finger-like projections in the small intestine called villi. These villi are responsible for absorbing nutrients. When they’re damaged, the body can’t absorb vitamins, minerals, or fats properly. But here’s the twist: that damage doesn’t stop at the gut. The liver is the body’s main filter. It processes everything that comes from the intestines through the portal vein. When the gut lining becomes leaky from celiac damage, toxins, bacteria, and undigested food particles slip into the bloodstream and head straight to the liver. The liver tries to clean it up, but over time, this constant bombardment causes inflammation. That’s why liver enzymes like ALT and AST rise-your liver is signaling stress. Studies show that 36.7% of people with celiac disease have abnormal liver enzymes at diagnosis, compared to just 19.3% in people without the condition. In over 70% of those cases, both ALT and AST are elevated together. That pattern is a red flag. It’s not typical of alcohol-related liver damage or viral hepatitis. It’s a signature of celiac-related liver stress.The Liver Conditions Linked to Celiac Disease
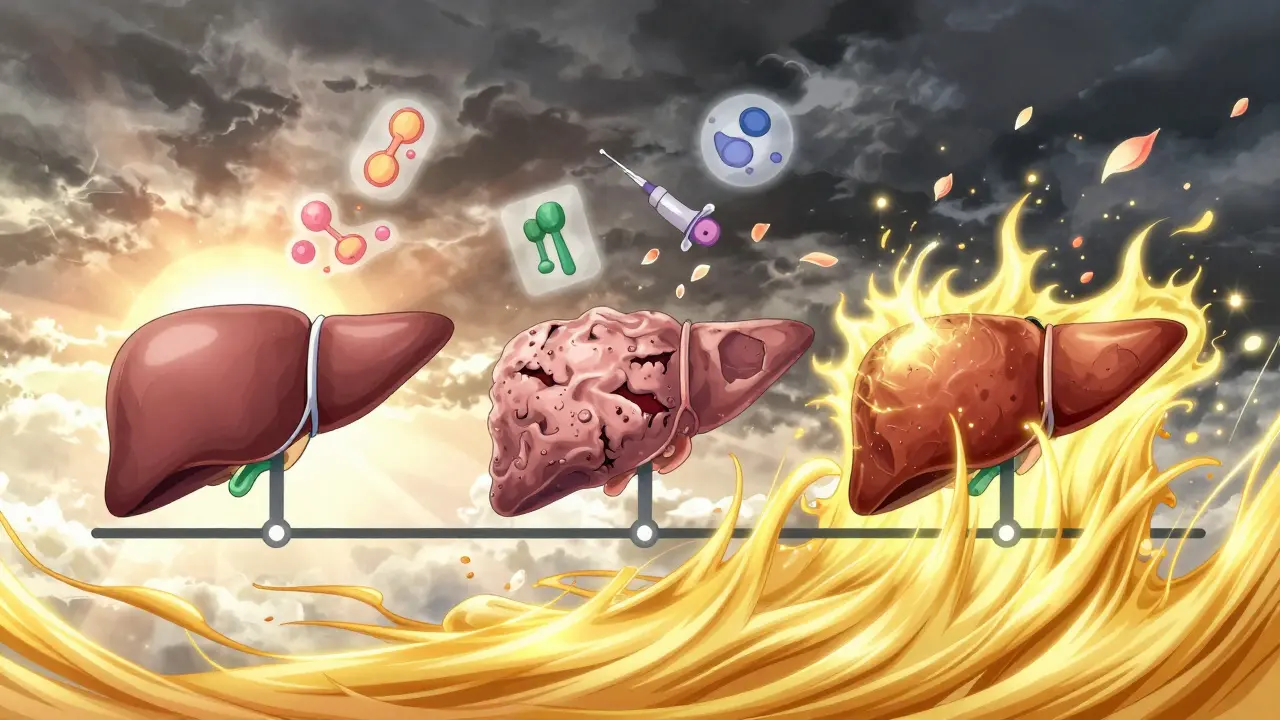
Celiac disease doesn’t just cause vague enzyme elevations. It’s tied to specific liver diseases:- Autoimmune hepatitis: About 4-6.4% of people with autoimmune hepatitis also have celiac disease. In some cases, the immune system attacks both the gut and the liver at the same time.
- Primary biliary cholangitis and primary sclerosing cholangitis: These rare conditions affect the bile ducts. People with celiac are more likely to develop them, though the exact link is still being studied.
- MASLD (metabolic dysfunction-associated steatotic liver disease): Once called fatty liver disease, MASLD is now recognized as a major complication. Surprisingly, it’s not always caused by obesity. In celiac patients, it can come from eating too many processed gluten-free foods-high in sugar, refined carbs, and unhealthy fats. These products replace wheat but don’t improve nutrition. They can trigger fat buildup in the liver, even in thin people.
The Glaring Paradox: Gluten-Free Diet Can Make Liver Problems Worse
Here’s the irony: the treatment for celiac disease-a gluten-free diet-can accidentally make liver issues worse. Many gluten-free products are loaded with corn syrup, potato starch, and hydrogenated oils. They’re cheaper to make and taste better, but they’re nutritionally empty. People with celiac often feel better after going gluten-free, so they start eating more of these processed foods. They gain weight. Their triglycerides climb. Fat builds up in the liver. A 2023 study found that celiac patients who ate mostly processed gluten-free foods were 3.2 times more likely to develop MASLD than those who ate whole foods like vegetables, lean meats, legumes, quinoa, and brown rice. The diet that saves your gut can harm your liver-if it’s not done right.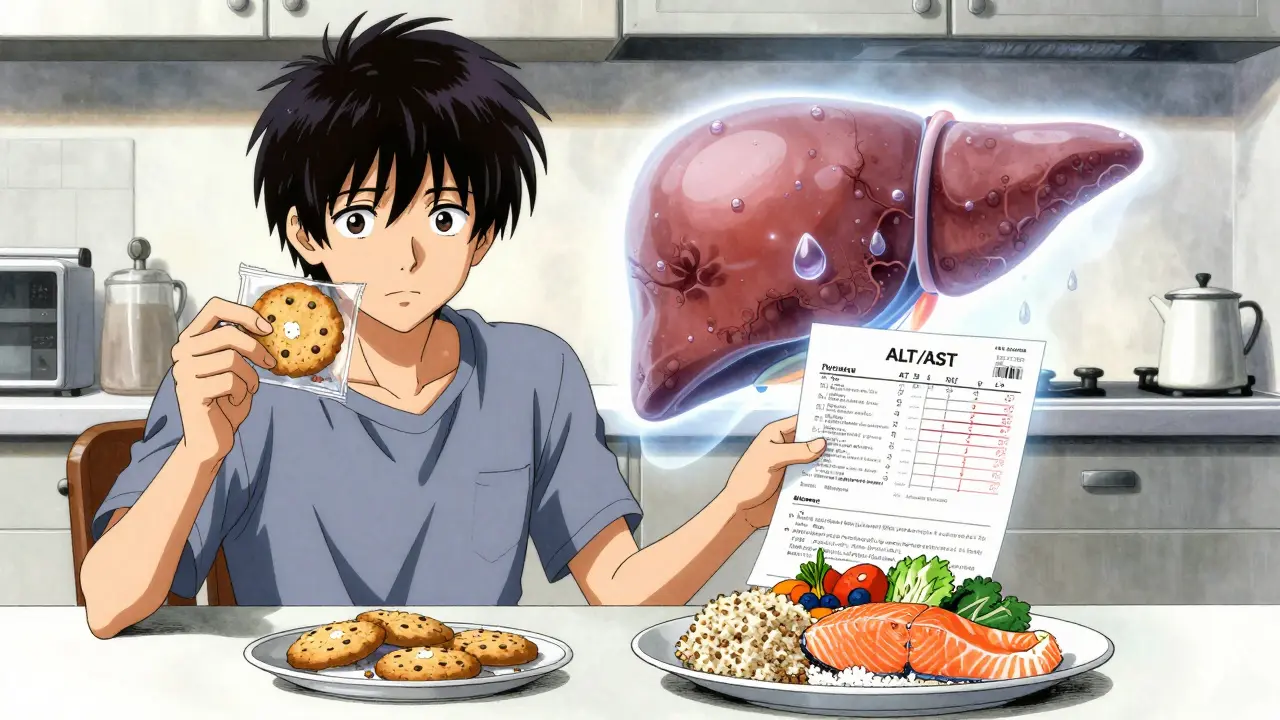
How Often Do Liver Enzymes Return to Normal?
The good news? For most people, the liver heals when gluten is removed. Research from Dr. Daniel Leffler at Beth Israel Deaconess Medical Center shows that 79% of celiac patients with elevated liver enzymes see their numbers return to normal within 12 to 18 months of strictly avoiding gluten. In 85% of cases, improvement happens within a year. That’s faster than most other liver conditions. Viral hepatitis or alcoholic liver disease require years of treatment. Celiac-related liver damage? Often fixed by one simple change: no gluten. But here’s the catch: it has to be strict. Even small amounts of gluten-like cross-contaminated oats or a bite of bread at a party-can keep liver enzymes high. One patient on a Reddit forum shared that her ALT was 142 at diagnosis. Doctors assumed fatty liver. Only after testing positive for tTG antibodies did they realize it was celiac. After six months of a clean gluten-free diet, her ALT dropped to 31.What to Do If Your Liver Enzymes Are High
If you’ve been told your liver enzymes are elevated and no cause has been found, ask for a celiac disease test. It’s simple: a blood test for tTG-IgA antibodies, followed by a biopsy if needed. Don’t wait. The longer you go untreated, the more damage builds up. If you’re already diagnosed with celiac and your liver enzymes are still high after a year of gluten-free eating, it’s time to dig deeper. You might have an autoimmune liver disease like autoimmune hepatitis. Or you might be eating too many processed gluten-free foods. Here’s what to do next:- Get a full liver panel: ALT, AST, ALP, GGT, bilirubin, albumin.
- Test for celiac antibodies (tTG-IgA, EMA, DGP) if you haven’t already.
- See a dietitian who specializes in celiac disease. They’ll help you switch from gluten-free junk food to real, whole foods.
- Get a liver ultrasound or FibroScan if enzymes stay high. It checks for fat or scarring.
- Rule out other causes: hepatitis B and C, alcohol use, medications, thyroid issues.
What Doctors Are Doing Differently Now
Ten years ago, liver tests weren’t routinely checked for celiac patients. Now, 92% of clinics include them in the initial workup. That’s a big shift. Why? Because researchers found that 4.7% of people with unexplained cirrhosis-liver scarring with no clear cause-had undiagnosed celiac disease. Once they went gluten-free, their liver function improved. In June 2024, the European Association for the Study of the Liver updated its guidelines. Now, they recommend testing for celiac disease in anyone with cryptogenic cirrhosis. That’s a major step. It means doctors are starting to see celiac not just as a gut disorder, but as a systemic disease that can damage the liver.How to Protect Your Liver While Going Gluten-Free
A gluten-free diet isn’t enough if it’s full of chips, cookies, and frozen meals. To protect your liver:- Focus on whole foods: vegetables, fruits, eggs, fish, chicken, beans, lentils, quinoa, rice, buckwheat.
- Avoid gluten-free baked goods made with white rice flour or tapioca starch-they spike blood sugar and feed liver fat.
- Limit added sugars. Read labels. If sugar is in the top three ingredients, skip it.
- Get enough vitamin E and omega-3s. They help reduce liver inflammation. Good sources: almonds, sunflower seeds, salmon, flaxseeds.
- Exercise regularly. Even 30 minutes of walking daily helps reduce liver fat.
The Bigger Picture: Why This Matters
Celiac disease isn’t just about avoiding bread. It’s a systemic immune disorder that can affect the liver, bones, nerves, skin, and brain. The liver connection is one of the most common and reversible extraintestinal manifestations. Yet, it’s still overlooked. If you have celiac disease and your liver enzymes are high, you’re not alone. And you don’t need more pills or procedures. You need a clean diet, time, and patience. Your liver can heal-often completely. The real challenge isn’t finding the cause. It’s changing how we think about celiac disease. It’s not a diet. It’s a lifelong immune condition. And your liver is one of the organs paying the price.Can celiac disease cause permanent liver damage?
In most cases, no. If celiac disease is diagnosed early and a strict gluten-free diet is followed, liver enzymes usually return to normal within a year. Liver biopsies show that fat accumulation and even mild scarring often reverse. However, if celiac disease remains undiagnosed for many years-especially with ongoing gluten exposure-there’s a risk of developing fibrosis or cirrhosis. That’s why early testing matters.
Do all people with celiac disease have liver problems?
No. About 15-40% of untreated celiac patients have elevated liver enzymes, but many have no symptoms. Some never develop any liver issues at all. However, even those with normal enzyme levels can still have early liver changes that show up on a biopsy. That’s why screening is recommended for everyone diagnosed with celiac disease.
Can a gluten-free diet reverse fatty liver in celiac patients?
Yes-if the fatty liver is caused by celiac-related malabsorption or inflammation. But if it’s caused by eating too many processed gluten-free foods high in sugar and fat, then simply removing gluten isn’t enough. You must also switch to whole, unprocessed foods. Studies show that patients who eat clean gluten-free diets see fat reduction in the liver within 6-12 months. Those who rely on gluten-free snacks often don’t improve.
Should I get tested for celiac disease if I have unexplained high liver enzymes?
Absolutely. If your liver enzymes are high and doctors can’t find a cause-like alcohol, hepatitis, or obesity-you should be tested for celiac disease. Up to 4.7% of people with unexplained cirrhosis have undiagnosed celiac. The test is a simple blood draw. If positive, starting a gluten-free diet can reverse liver damage and prevent future complications.
How long does it take for liver enzymes to normalize after going gluten-free?
Most people see improvement within 3-6 months. By 12 months, 85% have normal levels. By 18 months, 79% are fully normalized. But if enzymes haven’t improved after a year, you need further testing. You might have another liver condition, like autoimmune hepatitis, or you might still be exposed to gluten through hidden sources.

Timothy Davis
January 27, 2026 AT 12:51Let’s cut through the noise: elevated liver enzymes in celiac patients aren’t ‘mysterious’-they’re a direct consequence of intestinal permeability and endotoxin overload. The portal vein dumps everything from a leaky gut straight into the liver. ALT/AST elevations? Classic hepatocellular stress. The 36.7% stat? Spot on. But nobody talks about the fact that GGT and ALP often rise too-bile duct involvement is underreported. And yes, MASLD in celiac isn’t about obesity-it’s about fructose from corn syrup in gluten-free bread. Processed GF foods are the silent killer here. Studies from 2021 show even ‘clean’ GF diets with high glycemic load trigger de novo lipogenesis. Stop blaming the liver. Blame the food industry.
Howard Esakov
January 28, 2026 AT 06:30Wow, finally someone with actual science 🙄. I’ve been screaming this for years. People think ‘gluten-free’ = healthy. LOL. My cousin went GF and started eating nothing but gluten-free pizza rolls and rice cakes. Liver enzymes went from 80 to 210 in 8 months. She thought she was ‘eating clean.’ Bro, you’re just swapping wheat for high-fructose corn syrup and hydrogenated oils. The liver doesn’t care if it’s gluten-it cares about sugar, fat, and toxins. Also, if you’re not eating veggies, you’re just doing it wrong. 🤦♂️
Bryan Fracchia
January 29, 2026 AT 12:24This is one of those posts that makes you pause and rethink everything you thought you knew. I used to think celiac was just about avoiding bread. Turns out, it’s about relearning how to eat entirely. The part about processed gluten-free foods making liver damage worse? That hit me hard. I’ve been on a GF diet for 3 years and didn’t realize I was eating mostly junk. I’m switching to whole foods now-quinoa, lentils, veggies, nuts. No more GF cookies. It’s not about restriction, it’s about nourishment. And honestly? My energy’s already better. The liver can heal. We just have to give it the right fuel.
Lance Long
January 29, 2026 AT 18:24OH MY GOODNESS. I just read this and I’m crying. Not because it’s sad-but because it’s SO TRUE. I was diagnosed with celiac 5 years ago, and my ALT was 190. Doctors kept saying ‘fatty liver, lose weight.’ I was thin. I was confused. Then I found out it was celiac. I went gluten-free… and kept eating GF pasta, GF muffins, GF ice cream. My liver didn’t improve. Then I met a dietitian who said, ‘You’re not healing because you’re still poisoning yourself.’ I switched to real food. Broccoli. Salmon. Eggs. Sweet potatoes. Six months later? My ALT was 38. I didn’t need pills. I didn’t need surgery. I just needed to stop eating garbage disguised as ‘healthy.’ If you’re reading this and your liver’s still off-change your plate. Not just your diet. Your plate. You can heal. I did.
fiona vaz
January 30, 2026 AT 14:22Great breakdown. I’m a registered dietitian specializing in celiac, and I see this exact pattern every week. The liver normalization timeline is accurate-most patients see improvement by 6 months if they’re truly strict. But the biggest hurdle? Social eating. People think ‘gluten-free’ means ‘I can eat whatever as long as it’s labeled GF.’ Nope. The real healing comes from whole foods, not processed substitutes. I always tell my clients: if it comes in a bag with more than 5 ingredients you can’t pronounce, put it back. Your liver will thank you.
Sue Latham
January 30, 2026 AT 22:44Ugh, I’m so tired of people thinking gluten-free = automatically healthy. It’s 2024. We’ve known for a decade that GF junk food is worse than regular junk food. Sugar, fat, sodium-same problem, different label. And now the liver connection? Of course. Your gut’s leaking, your liver’s doing overtime. It’s not magic, it’s biology. If you’re not eating vegetables, you’re not healing. Plain and simple. Stop buying GF crackers and start buying kale. Your liver doesn’t care about your Instagram diet pics-it cares about what you actually swallow.
James Dwyer
February 1, 2026 AT 09:19I had elevated enzymes for two years. No one could figure it out. Then I got tested for celiac on a whim. Positive. Went gluten-free. Within 8 months, my ALT dropped from 156 to 34. No meds. No supplements. Just no gluten. If you’re reading this and your liver’s weird-get tested. It’s one blood test. Could save your life.
jonathan soba
February 1, 2026 AT 22:45Interesting, but you’re missing a key confounder: vitamin D deficiency. Celiac patients are notoriously deficient, and low D is independently linked to elevated liver enzymes and increased fibrosis risk. The 79% normalization rate? Likely higher in those who supplement. Also, zinc and magnesium status affects liver repair. The diet is critical-but micronutrients are the unsung heroes. Most dietitians overlook this. A gluten-free diet alone isn’t enough. You need targeted supplementation. Otherwise, you’re healing with one hand tied behind your back.