Many people think if a medicine makes them feel sick, they’re allergic to it. But that’s not always true. In fact, most of the time, it’s not an allergy at all-it’s just a side effect. And confusing the two can cost you more than just discomfort. It can lead to worse treatments, higher bills, and even dangerous infections. Understanding the real difference between side effects and allergic reactions isn’t just helpful-it’s life-saving.
What Are Medication Side Effects?
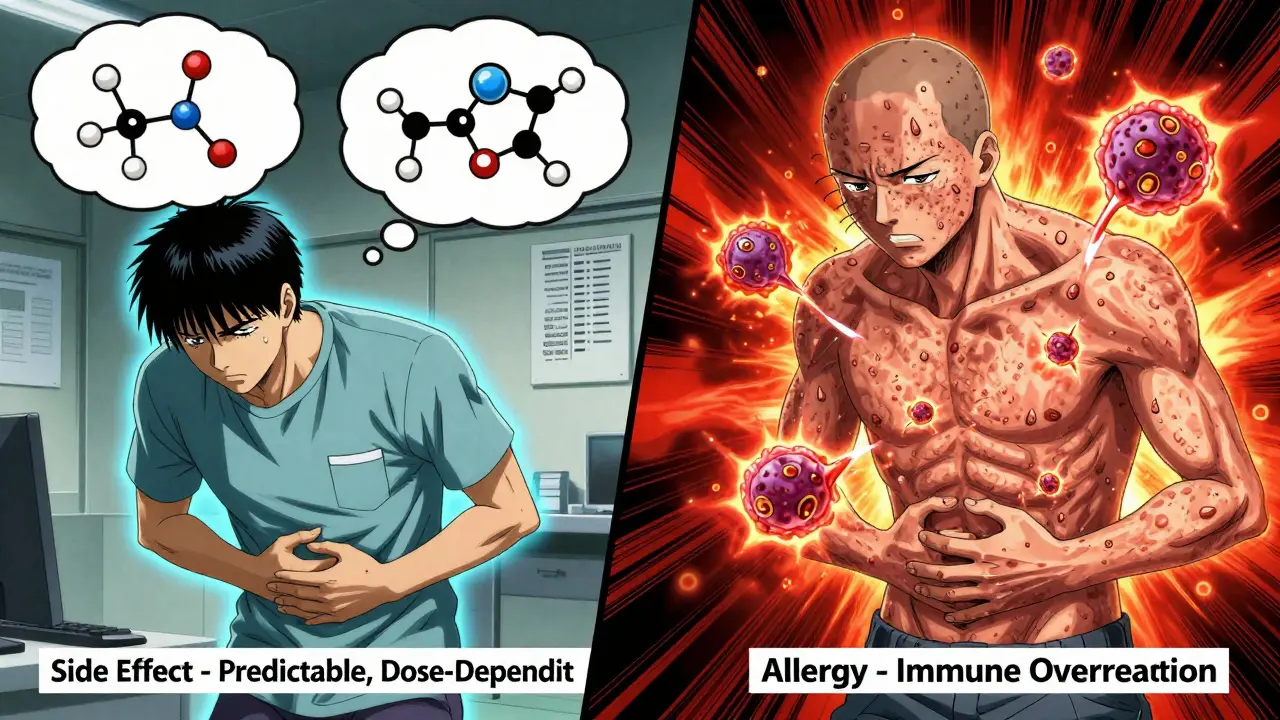
Side effects are predictable, known reactions to a drug’s chemical action in your body. They’re listed in the medication guide because they happen often enough to be documented. For example, statins-medicines for cholesterol-cause muscle aches in 5 to 10% of users. Metformin, used for diabetes, gives about 20 to 30% of people stomach upset. These aren’t random. They’re tied directly to how the drug works. These reactions usually show up within hours or days of starting the medicine. And here’s the good part: most of them fade over time. Around 70 to 80% of common side effects like nausea, dizziness, or mild fatigue disappear after two to four weeks as your body adjusts. That’s why doctors often tell you to keep taking the medicine even if you feel a little off at first. Side effects are also dose-dependent. Take more of an NSAID like ibuprofen, and your risk of stomach bleeding goes up. Take less, and the problem may go away. Sometimes, simple fixes help: taking metformin with food cuts GI issues in 60% of people. You don’t need to stop the drug-you just adjust how you take it.What Is a True Drug Allergy?
A drug allergy is completely different. It’s not about how the drug works-it’s about your immune system overreacting. Your body sees the medicine as an invader, like a virus or pollen, and launches an attack. This is why allergic reactions can be unpredictable and dangerous. There are two main types. Immediate reactions, triggered by IgE antibodies, happen within minutes to two hours. Symptoms include hives, swelling of the face or throat, trouble breathing, or a sudden drop in blood pressure. This is anaphylaxis-the most serious form. It’s rare, affecting only 0.05 to 0.5% of drug exposures, but it can be fatal if not treated right away. Delayed reactions take longer. Skin rashes like maculopapular eruptions show up one to two weeks after starting the drug. These are often T-cell mediated and can be mistaken for viral infections. In fact, 90% of these rashes develop within that window. The key difference? Side effects happen because of the drug’s chemistry. Allergies happen because your immune system is involved. And that changes everything.Why the Confusion Happens
People mix these up all the time. Why? Because symptoms can look similar. Diarrhea from amoxicillin? Many call it an allergy. A dry cough from lisinopril? They say they’re allergic. But neither is an allergy. A 2021 study in JAMA Internal Medicine found that 80 to 90% of people who say they’re allergic to penicillin aren’t. When tested properly, most turn out fine. Yet, they’re still labeled allergic in their medical records. That’s a problem. When doctors think you’re allergic to penicillin, they switch you to broader-spectrum antibiotics like vancomycin or ciprofloxacin. These drugs are stronger, more expensive, and disrupt your gut bacteria more. The result? A 69% higher chance of getting a dangerous infection like MRSA, according to Dr. Elina Jerschow of the American College of Allergy, Asthma & Immunology. In fact, mislabeled penicillin allergies cost the U.S. healthcare system over $1.1 billion a year. Each patient’s hospital stay gets longer by half a day to a full day. And that’s just one drug.
How Doctors Tell the Difference
There’s no single blood test that catches all allergies. But there’s a clear process. First, your doctor asks detailed questions: When did the reaction happen? What were the symptoms? Did you get worse with each dose? Was it immediate or delayed? This takes 15 to 20 minutes-and it’s the most important step. For penicillin, the CDC recommends a three-step approach:- Use a tool like PEN-FAST to assess your risk based on your history. About 60% of people can be cleared just by answering a few questions.
- Do a skin test. It’s 97% accurate at ruling out true IgE-mediated allergy.
- If the skin test is negative, do a small oral challenge under supervision. The chance of a reaction here is less than 0.2%.
What Happens If You’re Misdiagnosed?
The consequences are serious-and avoidable. If you’re wrongly labeled allergic to penicillin, you’re more likely to get a different antibiotic. That means higher risk of C. diff infection, longer hospital stays, and more antibiotic resistance. You might even be denied life-saving surgery because doctors won’t risk giving you the best drug. On the flip side, if you ignore a real allergy, you could end up in the ER. Anaphylaxis doesn’t wait. Hives, swelling, and trouble breathing? That’s not a side effect. That’s a medical emergency. Real stories show the difference. One woman on Drugs.com thought she was allergic to lisinopril because of a cough. Her doctor explained it was a known side effect, not an allergy. She switched to another blood pressure pill and felt fine. Another man, 28, had true anaphylaxis after his first penicillin dose-hives, swelling, and trouble breathing within 15 minutes. He now carries an epinephrine pen. One is a manageable side effect. The other is a life-threatening condition. Confusing them can change your health trajectory.
How to Protect Yourself
Here’s what you can do:- Don’t self-diagnose. If you feel sick after a new medicine, write down exactly what happened-timing, symptoms, duration.
- Ask your doctor: “Is this a side effect or could it be an allergy?”
- If you think you’re allergic to penicillin or sulfa drugs, ask about allergy testing. Most people don’t need to avoid these drugs forever.
- Update your medical records. If you were told you’re allergic but never tested, ask your doctor to review it. Many hospitals now have drug allergy clinics.
- Carry a list of your confirmed allergies. Don’t just say “allergic to antibiotics.” Be specific: “I have a true IgE-mediated allergy to amoxicillin.”
The Bigger Picture
This isn’t just about individual patients. It’s about public health. Mislabeling allergies leads to overuse of broad-spectrum antibiotics. That fuels drug-resistant superbugs. It’s one of the biggest threats to modern medicine. Hospitals that run allergy clarification programs have seen a 35% drop in unnecessary antibiotic use. The cost-benefit ratio? For every dollar spent on testing, you save $4.70 in avoided complications and longer stays. Yet, only 10% of U.S. allergists can handle the volume of patients needing evaluation. That’s why primary care doctors need better training. New tools in electronic health records now flag patients with unconfirmed allergies and prompt review. Early results show a 55% improvement in accurate documentation. The future is precision. Pharmacogenomics-testing your genes before prescribing-is already changing care for some drugs. More will follow.Final Takeaway
Not every bad reaction is an allergy. Most aren’t. But every real allergy deserves respect. The difference between a side effect and an allergic reaction isn’t just medical jargon-it’s the line between safe treatment and life-threatening risk. If you’ve ever said, “I’m allergic to this drug,” pause. Ask: What exactly happened? When? How bad? And most importantly-was it ever tested? You don’t need to live with a label you don’t deserve. And you don’t need to avoid a medicine that could save your life.Can a side effect turn into an allergy?
No, a side effect cannot turn into an allergy. Side effects are caused by the drug’s chemical interaction with your body, while allergies involve your immune system. One is pharmacological, the other immunological. They’re two different biological processes. However, you can develop a new allergy to a drug you’ve taken before-even if you never had a reaction before. That’s not a side effect turning into an allergy; it’s your immune system developing a new response.
Is a rash always a sign of a drug allergy?
Not always. Many rashes from medications are side effects, not allergies. For example, a mild, flat, red rash that appears one to two weeks after starting a drug is often a delayed T-cell reaction, which can be allergic-but not always. Other rashes are viral in origin and coincidentally appear after taking medicine. Only about 5 to 10% of all drug-related rashes are true allergic reactions. A doctor can help determine the cause using timing, symptoms, and sometimes skin or blood tests.
Can you outgrow a drug allergy?
Yes, especially with penicillin. Studies show that up to 80% of people who had a true penicillin allergy in childhood lose the sensitivity after 10 years. That’s why it’s important to get retested, especially if you were labeled allergic decades ago. Skin testing or an oral challenge under medical supervision can confirm whether you still react. Don’t assume you’re still allergic just because you were told so years ago.
What should I do if I think I’m allergic to a drug?
Don’t stop taking the medicine without talking to your doctor. Write down exactly what happened-timing, symptoms, how long it lasted. Then schedule an appointment to review it. If it’s a common drug like penicillin, ask about allergy testing. Many hospitals offer drug allergy clinics. Even if you’ve never been tested, you may still be able to safely use the drug. Don’t let an old label limit your treatment options.
Are over-the-counter drugs like ibuprofen commonly allergenic?
NSAIDs like ibuprofen can cause allergic reactions, but they’re rare. More often, they cause side effects like stomach upset or headaches. True allergic reactions to NSAIDs usually involve breathing problems, hives, or swelling, especially in people with asthma. These are not dose-dependent like side effects-they can happen even with a small dose. If you’ve had a reaction, get it evaluated. Don’t assume it’s just an upset stomach.
Why do some people get side effects and others don’t?
It comes down to genetics, metabolism, and overall health. Some people process drugs faster or slower. Others have genetic variations that make them more sensitive. For example, a gene called CYP2D6 affects how people metabolize codeine and other painkillers. Some turn it into morphine quickly and get strong side effects. Others barely feel anything. Age, liver function, and other medications also play a role. Side effects aren’t random-they’re individual.

Lindsey Kidd
December 23, 2025 AT 17:54Isaac Bonillo Alcaina
December 24, 2025 AT 16:31Bhargav Patel
December 26, 2025 AT 15:05Steven Mayer
December 28, 2025 AT 06:27Charles Barry
December 29, 2025 AT 02:12Rosemary O'Shea
December 29, 2025 AT 08:53Joe Jeter
December 30, 2025 AT 03:26Sidra Khan
December 30, 2025 AT 23:39Lu Jelonek
December 31, 2025 AT 07:01Ademola Madehin
December 31, 2025 AT 13:40suhani mathur
January 1, 2026 AT 03:12bharath vinay
January 2, 2026 AT 13:23Delilah Rose
January 3, 2026 AT 18:05Spencer Garcia
January 4, 2026 AT 05:53