Digoxin Bone Health Risk Assessment Tool
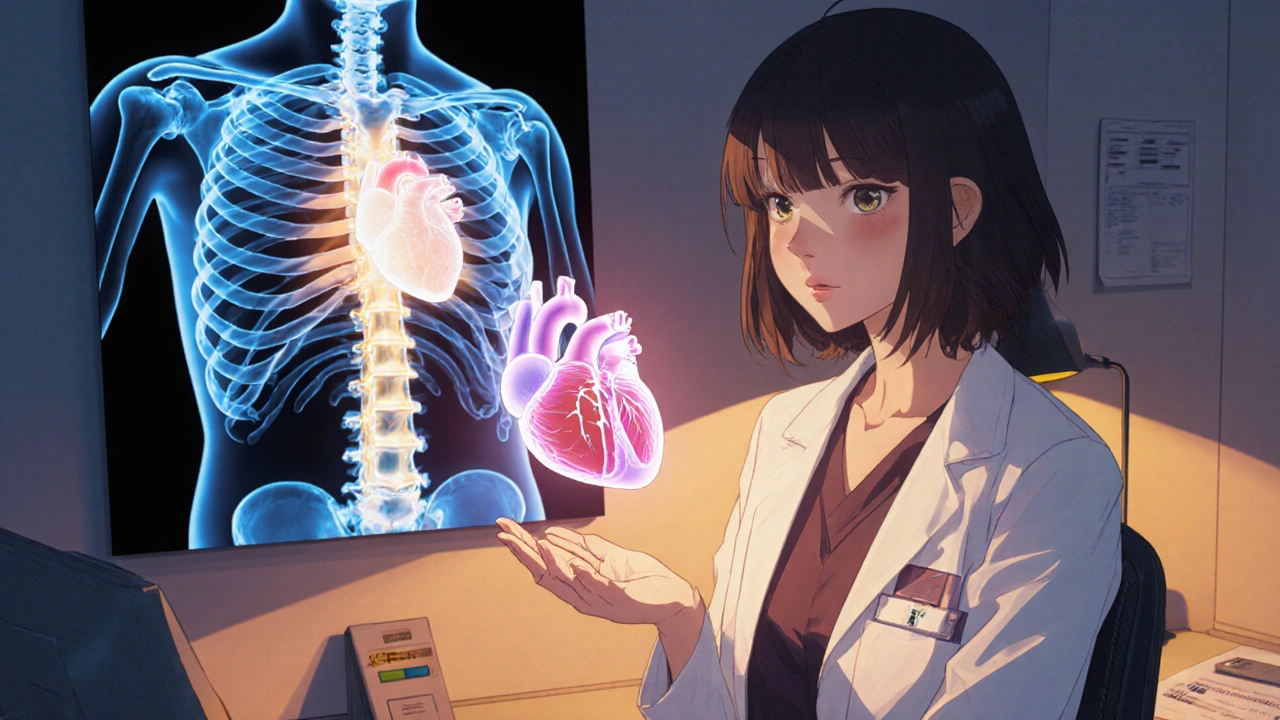
When you hear the word Digoxin is a cardiac glycoside that’s been used for decades to manage atrial fibrillation and heart failure. But a growing body of research asks a different question: does digoxin have any impact on bone health?
Key Takeaways
- Observational studies link long‑term digoxin use with modest changes in bone mineral density (BMD), especially in older women.
- Mechanistic data suggest digoxin may affect calcium handling through inhibition of Na+/K+ ATPase, which in turn influences osteoblast activity.
- Randomised trials are scarce; the few that exist show no clear clinical benefit or harm, leaving clinicians in a grey zone.
- Patients with renal impairment or high serum digoxin level should be monitored closely for both cardiac and skeletal side‑effects.
- Current guidelines do not address bone outcomes, so individual risk assessment remains essential.
What Is Digoxin?
First approved in the 1930s, digoxin works by inhibiting the Na+/K+ ATPase pump on cardiac myocytes. This inhibition raises intracellular sodium, which indirectly boosts calcium influx via the Na+/Ca2+ exchanger, strengthening heart contractions. The drug’s narrow therapeutic window means clinicians routinely check serum digoxin level to avoid toxicity.
Why Look at Bone Health?
Bone is a dynamic tissue constantly remodeling through the actions of osteoblasts (building) and osteoclasts (resorbing). Calcium balance, regulated by hormones like parathyroid hormone (PTH) and vitamin D, is central to this process. Any drug that interferes with calcium flux-like digoxin-could theoretically tip the remodeling scale.
Evidence from Observational Studies
Large cohort analyses in the United States and Europe have examined digoxin users versus non‑users for changes in bone mineral density (BMD). One 2022 study of 12,000 seniors reported a 2‑3 % lower lumbar spine BMD after five years of continuous digoxin therapy, particularly in post‑menopausal women. Another Danish registry linked digoxin to a 15 % higher odds of osteoporotic fracture, but the confidence interval barely crossed 1.0, suggesting a weak association.
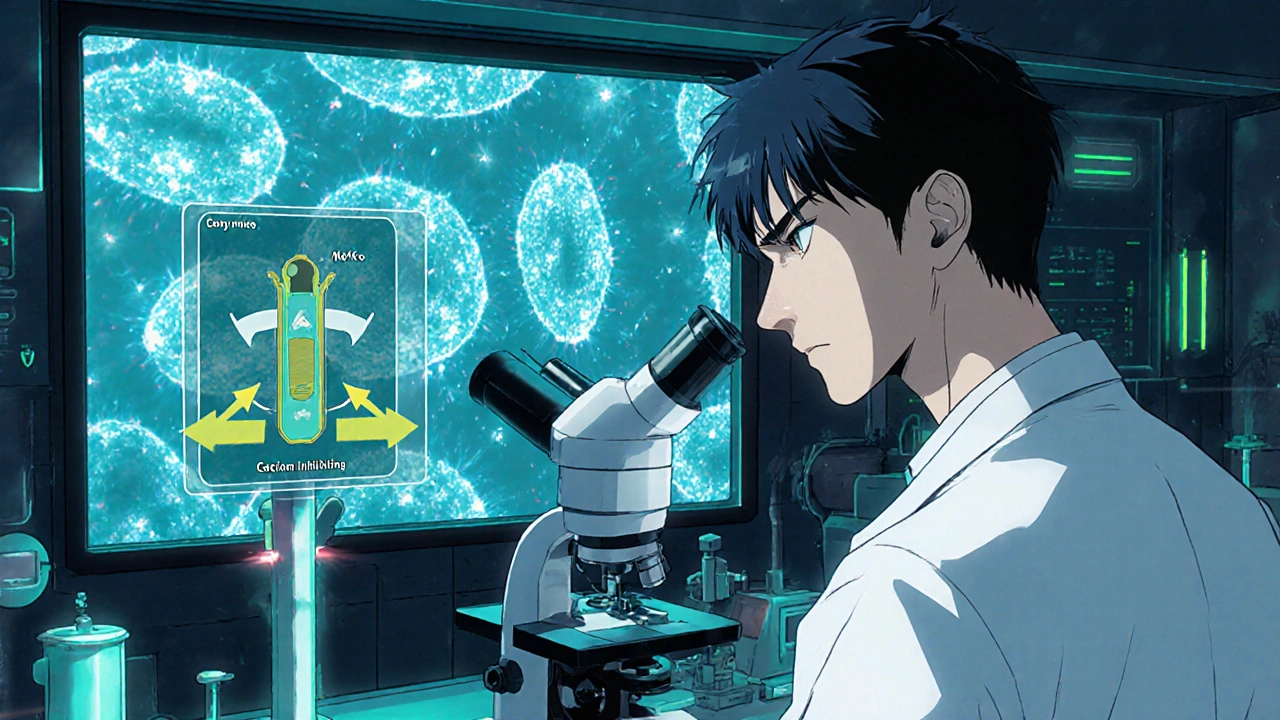
Mechanistic Insights
Laboratory work provides a plausible pathway. In vitro, digoxin reduces the activity of osteoblasts by dampening intracellular calcium spikes, which are essential for the expression of bone‑forming genes like COL1A1 and RUNX2. Conversely, osteoclasts appear less sensitive to digoxin, leading to an imbalance that favors resorption. Animal models (e.g., ovariectomised rats) given digoxin showed a slight drop in trabecular thickness after eight weeks.
Randomised Controlled Trials: The Gold Standard
Only two small RCTs have directly tackled the question. The first, a 2018 German pilot with 80 heart‑failure patients, randomised participants to low‑dose digoxin (0.125 mg) or placebo for 12 months. BMD measured by DXA showed no statistically significant difference, although the digoxin arm had a non‑significant trend toward lower femoral neck density.
The second trial, conducted in Japan in 2021, involved 102 elderly women with chronic atrial fibrillation. Participants received either standard digoxin dosing or a digoxin‑free regimen. After 18 months, fracture incidence was comparable, and lumbar spine BMD remained unchanged. Both studies were underpowered for definitive conclusions, leaving the field awaiting larger trials.
Clinical Implications for Practitioners
Given the mixed data, here are practical steps for clinicians managing patients on digoxin:
- Assess baseline bone risk. Use FRAX or a similar tool, especially in women over 65.
- Check renal function regularly-impaired kidneys raise both digoxin toxicity and bone turnover.
- Monitor serum digoxin level to stay within the 0.5-2.0 ng/mL therapeutic window.
- Consider calcium and vitamin D supplementation if BMD is borderline; this may offset any subtle negative impact.
- If a patient presents with unexplained fractures, review digoxin dosage and duration as part of the differential.
Patient Perspective: What Should You Know?
If you’re taking digoxin, don’t panic. The majority of users never experience bone problems. However, staying proactive helps. Ask your doctor about a baseline DXA scan if you’re over 60, maintain a diet rich in calcium (dairy, leafy greens) and vitamin D (sunlight, fortified foods), and keep active with weight‑bearing exercise.
Summary of Key Research Findings
| Study | Design | Population | Bone Outcome Measured | Result |
|---|---|---|---|---|
| US Cohort 2022 | Prospective observational | 12,000 adults >65 | Lumbar spine BMD (DXA) | −2‑3 % after 5 yr digoxin use |
| Denmark Registry 2020 | Case‑control | 7,800 heart‑failure patients | Osteoporotic fracture incidence | 15 % higher odds (borderline CI) |
| German RCT 2018 | Randomised, placebo‑controlled | 80 HF patients | Femoral neck BMD | No significant difference |
| Japanese RCT 2021 | Randomised, digoxin‑free arm | 102 elderly women with AF | Fracture rate & lumbar BMD | Comparable outcomes |
Future Directions
Researchers are now exploring digitised health records to perform large‑scale, propensity‑matched analyses that could finally settle the bone‑safety question. Meanwhile, a multi‑center RCT (NCT04876543) slated to start in 2026 aims to enrol 1,500 participants and directly measure fracture outcomes over three years. Until those results appear, clinicians must balance the proven cardiac benefits of digoxin against the tentative skeletal risks.
Frequently Asked Questions
Does digoxin cause osteoporosis?
Current data show a weak association, not a direct cause‑effect. Most studies report only modest BMD reductions, and large trials have not confirmed a rise in fracture risk.
Should I stop digoxin if I’m worried about my bones?
No. Digoxin’s cardiac benefits usually outweigh the uncertain bone risks. Talk to your doctor about possible bone‑protective measures instead of stopping the drug.
Are there alternative heart‑failure drugs that are safer for bone?
Beta‑blockers, ACE inhibitors, and ARNI agents have no known adverse effect on bone density. However, each class has its own profile, so therapy must be individualized.
How often should I get a bone scan while on digoxin?
If you have risk factors (age >65, female, low BMI, prior fracture), a DXA every 2‑3 years is reasonable. Otherwise, follow standard population‑screening guidelines.
Can vitamin D supplements counteract any negative bone effects of digoxin?
Adequate vitamin D (800-1000 IU daily) supports calcium absorption and may offset minor shifts in bone turnover, but it does not specifically neutralise digoxin’s cellular actions.
Bottom line: The evidence linking digoxin bone health is still emerging. Keep an eye on your heart health, stay on top of bone‑screening if you’re at risk, and discuss any concerns with your healthcare provider.

Angela Koulouris
October 21, 2025 AT 15:03Great synthesis of the current digoxin‑bone data. Your recap paints a clear picture for clinicians juggling cardiac and skeletal concerns, and the colorful analogies make it easier to digest. I especially appreciate the practical checklist for monitoring patients over 65. Keep the useful nuggets coming!
Harry Bhullar
October 25, 2025 AT 02:23Let me break this down in detail because the nuances matter when we talk about cardiac glycosides and skeletal turnover. First, digoxin’s inhibition of Na⁺/K⁺‑ATPase leads to a cascade that raises intracellular sodium, indirectly modulating the Na⁺/Ca²⁺ exchanger and altering calcium homeostasis in both myocytes and osteoblasts. That shift can blunt the calcium spikes needed for RUNX2 activation, which in turn may dampen osteoblast differentiation and matrix deposition. The observational cohorts you cited show a modest 2‑3% lumbar spine BMD decline over five years, which aligns with the in‑vitro data where reduced COL1A1 transcription was noted. However, the confidence intervals in those studies are wide, and the Danish registry’s 15% increased fracture odds barely crossed the threshold of statistical significance, suggesting a potential type‑I error. Randomised trials are sparse; the German pilot, despite its rigorous double‑blind design, was underpowered to detect small BMD changes, and the Japanese study’s fracture rates were statistically indistinguishable between groups. Moreover, patient heterogeneity-differences in baseline vitamin D status, renal clearance, and concomitant bisphosphonate use-confounds any direct causal inference. From a mechanistic standpoint, animal models do show a slight reduction in trabecular thickness, but the effect size is modest and may not translate clinically. Clinicians should therefore individualise care: assess FRAX risk, ensure adequate calcium and vitamin D, and consider periodic DXA scans in high‑risk patients, especially post‑menopausal women with chronic digoxin exposure. Monitoring serum digoxin levels remains crucial, as supratherapeutic concentrations could exacerbate any adverse skeletal signaling. In summary, while there is a plausible biological pathway linking digoxin to bone remodeling, the current human data are insufficient to mandate changes in prescribing practices; vigilant risk assessment and bone health optimisation remain the best approach.
Dana Yonce
October 28, 2025 AT 12:43Nice overview 😊
Lolita Gaela
November 1, 2025 AT 00:03The pharmacodynamic profile of digoxin suggests a dualistic impact on the osteogenic niche via modulation of intracellular Ca²⁺ fluxes. Inhibitory action on Na⁺/K⁺‑ATPase attenuates the secondary activation of the Na⁺/Ca²⁺ exchanger, thereby curtailing the amplitude of calcium transients essential for osteoblastogenesis. Subsequent down‑regulation of osteogenic transcription factors such as RUNX2 and osterix compromises matrix mineralisation. Conversely, osteoclasts display relative insensitivity to these ionic perturbations, potentially skewing the remodeling balance toward resorption. This mechanistic paradigm aligns with the modest BMD decrements observed in epidemiologic cohorts, though causality remains to be definitively established.
Giusto Madison
November 4, 2025 AT 11:23Listen up, folks: if you’re on digoxin and worried about bones, the key is balance. Keep your calcium and vitamin D intake solid, get a DXA if you’re over 65, and don’t let the fear of a tiny BMD dip drive you off a life‑saving drug. Stay on top of serum levels, and you’ll dodge the worst of both worlds.
Xavier Lusky
November 7, 2025 AT 22:43It’s no coincidence that pharmaceutical giants push digoxin without disclosing its hidden skeletal agenda. The data are being quietly buried while they market it as a miracle for heart failure, all the while letting patients suffer unseen bone loss. Trust no one who washes their hands of the long‑term consequences.
Ashok Kumar
November 11, 2025 AT 10:03Ah, the classic “big pharma conspiracy” narrative-ripe for a sardonic eye roll. While it’s wise to stay skeptical, the studies you mention are peer‑reviewed and the mechanisms are biologically plausible, not some secret plot. Let’s keep the drama for reality TV, not for interpreting clinical data.
Esther Olabisi
November 14, 2025 AT 21:23Love the energy here 😎. If you’re on digoxin, consider a quick weekly walk, grab a glass of milk, and maybe a sunny afternoon-those tiny habits can keep both your heart and bones humming. 🌞💪
Ivan Laney
November 18, 2025 AT 08:43Patriots of medicine, hear me: our country's heart health shouldn’t be sacrificed on the altar of flimsy bone data imported from foreign registries. The American standard of care has always placed cardiac survival first, and digoxin remains a cornerstone in that hierarchy. Those European studies, while interesting, don’t overturn decades of domestic experience. Keep the focus on proven life‑saving therapies, and let the bone worries be a secondary, individualized concern.
Sakib Shaikh
November 21, 2025 AT 20:03Whoa, you're overdramatic! iT's nOt a disASTer whEn a lil bit oF bOne loss happenS, it 2.0k was only a mini. cALM DoN't blow iT uP, yoU knOw?
Devendra Tripathi
November 25, 2025 AT 07:23Actually, the whole premise that digoxin mildly affects bone is overrated. The evidence is weak, and the drug’s cardiac benefits far outweigh any theoretical skeletal risk. So, I’d say we’re fine.
Vivian Annastasia
November 28, 2025 AT 18:43Sure, because ignoring a potential side effect is always the best medical practice. 🙄 Let’s just pretend the bones are invincible when they’re not.
eric smith
December 2, 2025 AT 06:03Oh wow, another “expert” telling us what to do-because we obviously needed a lecture on calcium.
Erika Thonn
December 5, 2025 AT 17:23Philosopically, one might wonder if bone health is merely a metaphor for the structural integrity of our lives; yet, i think we should kepp checking our DXAs as a form of existential verification.
Jake Hayes
December 9, 2025 AT 04:43Bottom line: the data are inconclusive, so monitor and don’t abandon proven therapy.