DAPT Bleeding Risk Calculator
Assess Your Bleeding Risk
The PRECISE-DAPT score helps doctors identify patients at high risk for bleeding during dual antiplatelet therapy. Enter your risk factors below to see your score.
Your Bleeding Risk
Important: This tool is for informational purposes only. Your doctor will determine the appropriate duration and type of antiplatelet therapy based on your full medical history. Do not change your medication without consulting your healthcare provider.
When you’ve had a heart stent placed or survived a heart attack, doctors often prescribe dual antiplatelet therapy-a combo of aspirin and another drug like clopidogrel, prasugrel, or ticagrelor. It’s meant to stop clots from forming inside the stent and prevent another heart attack. But here’s the catch: the same drugs that save your heart can also make you bleed more easily. A small cut might take longer to stop. You might get nosebleeds. Or worse-internal bleeding that needs hospital care.
Why Dual Antiplatelet Therapy Works (and Why It’s Risky)
Dual antiplatelet therapy, or DAPT, blocks platelets-the tiny blood cells that clump together to form clots. After a stent is placed, your body sees it as an injury. Platelets rush in, and without DAPT, they can form a clot right inside the stent. That’s a medical emergency. DAPT cuts that risk by 15-30% compared to taking just one drug.
But platelets don’t just form clots where they shouldn’t. They’re also your body’s first responders to cuts, scrapes, and bruises. When you slow them down too much, even minor injuries turn into problems. Studies show that for every 100 people on DAPT, 1 to 2 will have a major bleeding event within a year. That’s not rare. It’s common enough that doctors now treat bleeding risk as seriously as clot risk.
Which Drugs Are Used-and How They Differ
DAPT always includes aspirin (75-100 mg daily). The second drug is where choices matter:
- Clopidogrel (75 mg daily): Older, cheaper, less powerful. Bleeding risk is lower, but it doesn’t prevent heart events as well as newer drugs.
- Prasugrel (10 mg daily): Stronger than clopidogrel. Better at preventing heart attacks, but increases bleeding risk by about 25%.
- Ticagrelor (90 mg twice daily): Most potent. Reduces heart attack and death rates more than clopidogrel, but causes 27% more major bleeding, according to clinical trials.
The 2023 European guidelines say ticagrelor and prasugrel are preferred for most patients-unless they’re at high risk for bleeding. Then, clopidogrel becomes the safer starting point.
Who’s at Highest Risk for Bleeding?
Not everyone on DAPT bleeds. But some people are far more likely to. Doctors use a tool called the PRECISE-DAPT score to measure this. A score of 25 or higher means you’re at high bleeding risk. You’re in that group if you have:
- Age 75 or older
- History of bleeding (even a simple nosebleed that needed treatment)
- Low hemoglobin (anemia)
- Chronic kidney disease (creatinine clearance under 60)
- Low platelet count
- Already taking a blood thinner like warfarin or apixaban
One in five PCI patients today meet these criteria. That’s up from just 15% in 2017. Hospitals are getting better at spotting them early.
What Does Bleeding Actually Look Like?
Most bleeding isn’t dramatic. It doesn’t always mean vomiting blood or passing out. More often, it’s:
- Nosebleeds that last longer than 10 minutes or happen more than once a week
- Bleeding gums when brushing teeth
- Unexplained bruises on arms or legs
- Dark, tarry stools (sign of stomach bleeding)
- Red or pink urine
- Heavy or prolonged menstrual bleeding
There’s also something called nuisance bleeding-minor bleeding that doesn’t need hospital care but makes you anxious. In one study, 15% of patients on ticagrelor had this within the first month. And here’s the real problem: 18.7% of those patients stopped taking their meds within six months because they were scared. That’s dangerous. Stopping DAPT too early doubles or triples your risk of stent clotting.
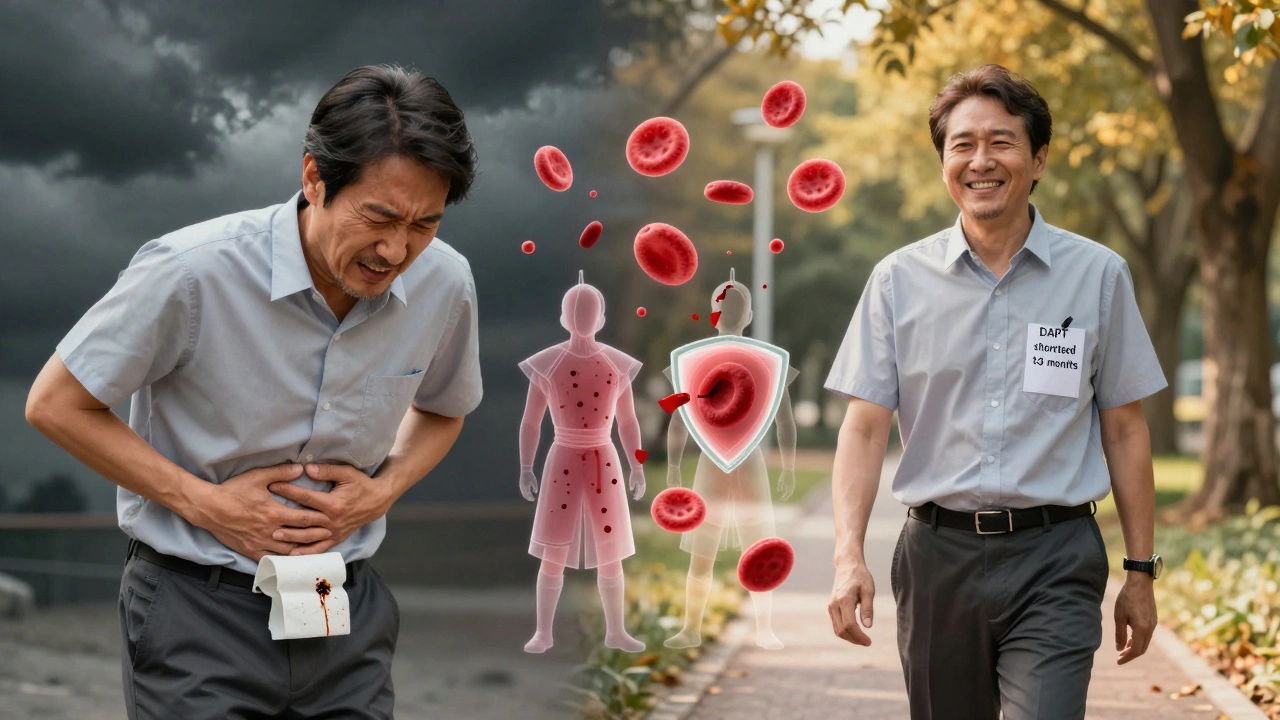
How Doctors Adjust Treatment to Reduce Bleeding
For years, everyone got 12 months of DAPT. Now, we know that’s too long for many. The goal isn’t just to prevent clots-it’s to prevent both clots and bleeding. Here’s how doctors are changing their approach:
- Shortening DAPT to 1 month: For high-risk patients, studies like MASTER DAPT show that stopping DAPT after just 1 month, then switching to aspirin alone, cuts major bleeding by nearly 7%-without raising heart attack risk.
- De-escalation: Start with ticagrelor or prasugrel for 1-3 months, then switch to clopidogrel. The TALOS-AMI trial found this reduced bleeding by 2.1% without increasing heart events.
- Stopping DAPT entirely after 6 months: For patients with low clot risk but high bleeding risk, guidelines now support stopping DAPT at 6 months if the stent is healed and there’s no history of clots.
One big mistake? Stopping DAPT on your own because you’re scared of bleeding. Always talk to your doctor first. Premature stopping can be deadly.
What to Do If You Start Bleeding
If you notice minor bleeding-like a nosebleed or gum bleeding-don’t panic. But do:
- Apply pressure for 10-15 minutes
- Avoid aspirin or NSAIDs like ibuprofen (they make bleeding worse)
- Call your doctor if it doesn’t stop or keeps coming back
For major bleeding-vomiting blood, black stools, sudden weakness, dizziness, or swelling in the abdomen-go to the ER immediately. Don’t wait. Hospitals have protocols. If you had a stent placed within the last 3 months, they’ll likely restart DAPT as soon as you’re stable. After 3-6 months, they might switch you to aspirin alone.
Platelet transfusions? Only used in life-threatening cases. And even then, they’re not a magic fix. One unit of platelets might restore only 30% of your clotting ability for a few hours.
What You Should Avoid
Some things make bleeding worse. Avoid them:
- NSAIDs: Ibuprofen, naproxen, diclofenac-these interfere with aspirin and increase stomach bleeding risk.
- Alcohol: More than one drink a day can thin your blood further and irritate your stomach lining.
- Herbal supplements: Garlic, ginkgo, ginseng, fish oil, and vitamin E can all increase bleeding risk. Tell your doctor about everything you take.
- Unnecessary procedures: You don’t need to stop DAPT for a dental cleaning, colonoscopy, or even a lumbar puncture. But always tell your dentist or doctor you’re on DAPT.
Quality of Life Matters
Bleeding doesn’t just hurt-it changes your life. In surveys, 68% of patients with minor bleeding said they worried constantly about getting hurt. 41% avoided social events because they didn’t want to bleed in public. That’s isolation. That’s fear.
But here’s good news: patients who switched from ticagrelor to clopidogrel reported a 15-point improvement in quality-of-life scores within six months. They slept better. They went out more. They felt in control again.
Managing bleeding isn’t about avoiding all risk. It’s about finding the right balance. The goal isn’t to never bleed. It’s to live without fear of bleeding.
What’s Next? The Future of DAPT
Doctors are moving toward personalization. No more one-size-fits-all. In 2023, a new NIH-funded registry called DAPT-PLUS started tracking 15,000 patients using AI to predict who will bleed and who won’t. By 2028, experts predict 90% of stent patients will get a custom DAPT plan-shorter, smarter, safer.
There’s also hope for reversal drugs. Right now, if you bleed badly on DAPT, there’s no quick antidote-unlike with blood thinners like warfarin or dabigatran. Two experimental drugs are already in early trials. They might be available by 2027.
For now, the best tool you have is communication. Talk to your doctor. Ask: “Am I high risk for bleeding?” “Can we shorten this?” “Can we switch to clopidogrel?” Your life depends on it-not just your heart, but your freedom to live without fear.
How long should I stay on dual antiplatelet therapy after a stent?
It depends on your risk. For most people, 6 to 12 months is standard. If you’re at high risk for bleeding, your doctor may recommend stopping after 1 or 3 months and switching to aspirin alone. If you’re at high risk for clots, you might need 12 months or longer. Never stop on your own-always talk to your doctor first.
Can I take ibuprofen or aspirin for headaches while on DAPT?
Don’t take ibuprofen, naproxen, or other NSAIDs. They increase your risk of stomach bleeding and can interfere with aspirin’s heart protection. For headaches, use acetaminophen (Tylenol) instead. Always check with your doctor before taking any new medication, even over-the-counter ones.
Is it safe to drink alcohol while on DAPT?
One drink a day is usually okay, but more than that increases bleeding risk, especially in the stomach. Alcohol can irritate your stomach lining and thin your blood. If you have a history of ulcers or liver disease, avoid alcohol completely. Always ask your doctor what’s safe for you.
What should I do if I start bleeding from a small cut?
Apply firm pressure with a clean cloth for at least 10-15 minutes. Don’t check frequently-it slows healing. If the bleeding doesn’t stop, or if you’re bleeding from multiple places, call your doctor. Don’t assume it’s normal. Even minor bleeding can be a sign you’re on too strong a dose.
Can I stop DAPT if I feel fine?
No. Feeling fine doesn’t mean you’re safe. Stopping DAPT too early-especially before 6 months-can cause a deadly clot inside your stent. That risk is 2-3 times higher if you quit early. Only stop if your doctor tells you it’s safe based on your individual risk.
Are there any tests to check if my DAPT is working right?
Platelet function tests exist, but major medical groups-including the French Working Group and ACC-say they’re not useful for routine care. There’s no clear proof they prevent bleeding or improve outcomes. Doctors rely on your symptoms, risk factors, and medical history instead.
What happens if I miss a dose of my antiplatelet drug?
If you miss one dose, take it as soon as you remember-unless it’s almost time for the next one. Don’t double up. Missing one dose isn’t usually dangerous, but regularly skipping doses increases clot risk. Set phone reminders or use a pill organizer. Consistency matters more than perfection.
Final Thought: It’s Not About Avoiding Bleeding-It’s About Managing It
Dual antiplatelet therapy isn’t perfect. But it’s one of the most effective tools we have to save lives after heart procedures. The key isn’t to avoid bleeding at all costs-it’s to manage it smartly. Work with your doctor. Know your risk. Ask questions. And don’t let fear make you stop taking your medicine. The goal isn’t to live without bleeding. It’s to live without fear.

Jennifer Blandford
December 7, 2025 AT 13:52Just had my stent last year and honestly? I thought I’d be terrified forever. Turns out, I just needed to know what ‘minor bleeding’ actually looked like. Now I don’t panic when my gums bleed a little. This post saved my sanity. 🙏❤️
Rich Paul
December 8, 2025 AT 16:01tfw you take ticagrelor and your doc says ‘just chill’ but then you get a nosebleed and suddenly you’re googling ‘can platelets die from stress’ 😭
Ruth Witte
December 9, 2025 AT 11:47YOU ARE NOT ALONE. I stopped my meds for 3 days because I was scared of bruising. My cardiologist nearly had a heart attack. Don’t be me. 😅
Katherine Rodgers
December 9, 2025 AT 16:16So let me get this straight… we’re giving people drugs that turn them into glass people, then telling them ‘just don’t get hurt’? Brilliant. 🤡
Lauren Dare
December 11, 2025 AT 00:17PRECEISE-DAPT score? More like PRECISE-DOCTOR-TOOK-20-MINUTES-TO-EXPLAIN-THIS score. I still don’t know if I’m high risk or just unlucky. 😒
Steve Sullivan
December 12, 2025 AT 04:16It’s wild how we treat clotting like a horror movie and bleeding like a minor inconvenience. But the truth? Bleeding steals your life slower, but just as surely. You stop going out. Stop hugging your grandkids. Stop feeling safe in your own skin. This isn’t just pharmacology - it’s psychological warfare. 🤯
Raja Herbal
December 13, 2025 AT 18:43So if I’m 78, anemic, and on warfarin… I’m basically a walking bleeding time bomb? Cool. Thanks for the clarity, doc. 🙃
Gilbert Lacasandile
December 14, 2025 AT 07:34My wife switched from ticagrelor to clopidogrel last month. She’s sleeping through the night for the first time in a year. No more jumping at every cough. I didn’t realize how much fear was weighing her down. This isn’t just medicine - it’s peace of mind.
Asset Finance Komrade
December 15, 2025 AT 04:11One must question the ontological basis of DAPT: if platelets are the agents of both life and death, then is the body not already a paradox? We intervene not to heal, but to balance the tension between two fundamental forces - coagulation and hemorrhage - as if the human form were a chemical equation. The real question: who decided that bleeding was the lesser evil? And why do we call it ‘risk management’ when it feels more like surrender?
Graham Abbas
December 17, 2025 AT 02:51There’s a quiet dignity in learning to live with vulnerability. I used to think ‘being strong’ meant never bleeding. Now I know it means showing up anyway - even when your gums bleed, even when you’re scared. This isn’t about drugs. It’s about courage in the daily grind.
Nikhil Pattni
December 18, 2025 AT 08:32Okay but let’s be real - if you’re on DAPT and you’re not taking ginkgo, garlic, fish oil, vitamin E, and a shot of whiskey every morning, you’re doing it wrong. I’ve been on ticagrelor for 2 years, had 3 nosebleeds, and still hiked Machu Picchu. The real enemy? Doctors who scare you into compliance. You want to live? Take your meds and live like you mean it. Also, if your doctor says ‘avoid NSAIDs’ but doesn’t tell you about CBD oil - they’re not doing their job. CBD doesn’t thin blood like ibuprofen. Ask your pharmacist. I did. And now I sleep like a baby. 😴💊
Kathy Haverly
December 19, 2025 AT 04:54Wow. So the solution to bleeding risk is… switching to a weaker drug? What a shocker. Next they’ll tell us to stop wearing seatbelts to avoid bruising. This is just corporate medicine in a lab coat. Why not just give everyone aspirin and call it a day? Oh right - because the pharmaceutical industry needs to sell you $400 pills that ‘work better.’
Steve Sullivan
December 20, 2025 AT 00:03Just read this thread. To the person who said they switched to clopidogrel and slept better - I’m doing that next week. I’ve been on ticagrelor for 14 months. My wife says I’ve been ‘on edge’ since day one. Maybe it’s not just the stent. Maybe it’s the drug. Thanks for normalizing this. 🙏