When you’re pregnant, even a simple headache can turn into a panic. Should you take that painkiller? Is that cold medicine safe? The truth is, the first 12 weeks of pregnancy - the first trimester - are the most sensitive time for your baby’s development. This isn’t just a general warning. It’s a biological fact. Every pill, every drop, every substance you take during these weeks can influence how your baby’s organs form. And the window for major damage? It’s narrower than most people think.
Why the First Trimester Is So Critical
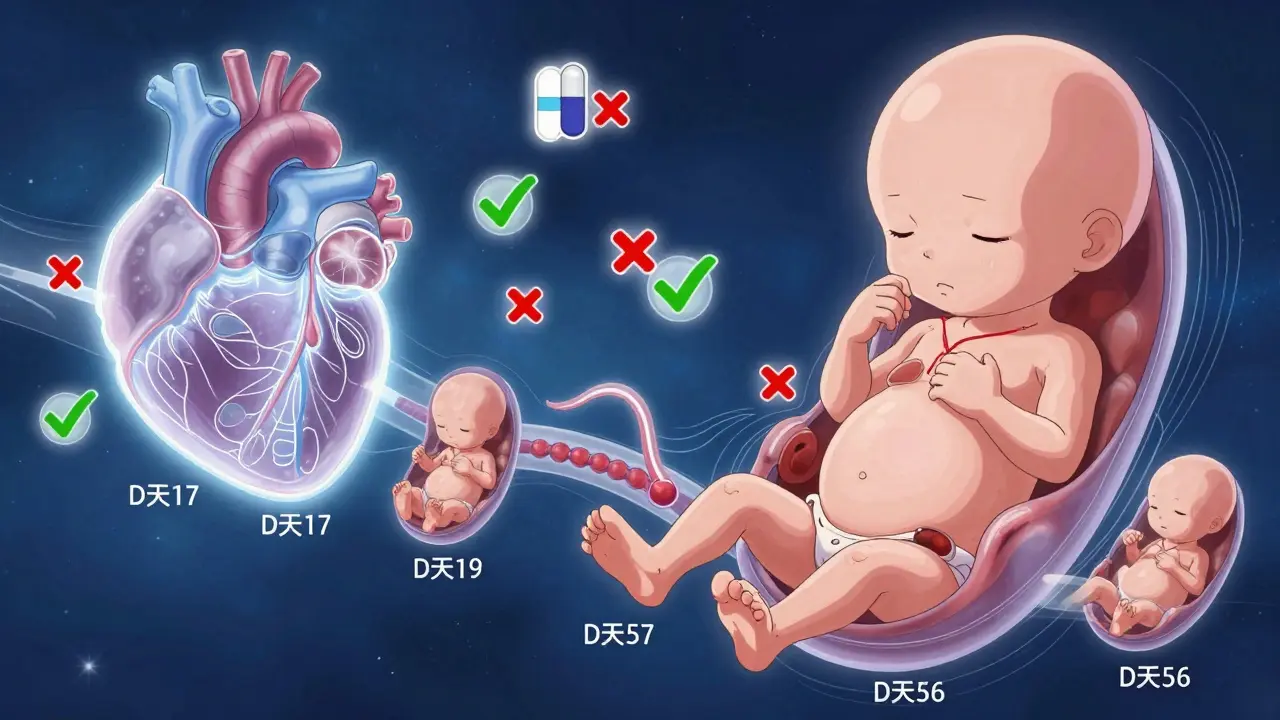
Your baby doesn’t start out as a tiny human. It starts as a cluster of cells. By week 3, those cells begin to organize into layers that will become every organ system. By week 8, the heart is beating, the brain is dividing into hemispheres, and the limbs are budding. By week 12, most major structures are in place. That’s why the period between days 17 and 56 after conception - roughly weeks 3 to 8 - is called the embryonic period. This is when your baby is most vulnerable to things that can cause birth defects.
Think of it like building a house. If you mess with the foundation or the framing during construction, the whole structure can be ruined. But once the walls are up, you can still fix a leaky roof. That’s the difference between the first trimester and later stages. The organs are being built. One wrong move - like taking a certain medication - can change how they form forever.
The CDC says about 90% of major birth defects happen during this time. Neural tube defects? That’s days 18 to 26. Heart problems? Days 20 to 40. Limb abnormalities? Days 24 to 36. Timing matters. And so does the drug.
Common Medications and Their Real Risks
Most pregnant people take at least one medication in the first trimester. Some because they’re managing chronic conditions. Others because they’re treating a cold, headache, or nausea. But not all medications are created equal.
Acetaminophen (Tylenol) has been the go-to for pain and fever for decades. It’s still considered the safest option. The recommended dose is up to 4,000 mg per day - that’s four 500 mg tablets. But new research is raising red flags. Studies now suggest that long-term or frequent use might be linked to a 30% higher risk of ADHD and a 20% higher risk of autism spectrum disorder. That doesn’t mean you can’t use it. It means you should use it only when needed, at the lowest dose, for the shortest time.
NSAIDs like ibuprofen, naproxen, and aspirin are a different story. They’re common, but dangerous in early pregnancy. A Canadian study of over 4,700 pregnancies found that taking NSAIDs in the first trimester increases the risk of miscarriage by 1.6 times. Even more concerning, they can interfere with the development of the baby’s heart and kidneys. The FDA warns against using them after 20 weeks - but the risk starts much earlier.
Antidepressants are another big concern. If you’re managing depression or anxiety, stopping your medication can be just as risky as continuing it. But not all SSRIs are the same. Paroxetine has been linked to a 1.5 to 2 times higher risk of heart defects, especially ventricular septal defects. That’s why doctors often switch you to sertraline or citalopram, which have no clear link to major birth defects. But even these can cause temporary withdrawal symptoms in newborns - called neonatal adaptation syndrome - if taken late in pregnancy.
Antibiotics are often needed. Amoxicillin, cephalosporins, and erythromycin are generally safe. But tetracycline stains developing teeth and weakens bones - so it’s off-limits after 15 weeks. Fluoroquinolones like ciprofloxacin damage cartilage in animal studies. Human data is limited, but most doctors avoid them unless there’s no other option.
What About Cold, Allergy, and Stomach Medicines?
Everyone gets sick. But what you reach for matters.
Pseudoephedrine (Sudafed) is a common decongestant. But a 2002 study found it might increase the risk of gastroschisis - a rare birth defect where the baby’s intestines develop outside the abdomen. The risk is small, but real. Most experts recommend avoiding it in the first trimester. Use saline sprays or humidifiers instead.
Antihistamines like diphenhydramine (Benadryl), loratadine (Claritin), and cetirizine (Zyrtec) are generally considered safe. But don’t assume all OTC allergy meds are okay. Always check the label. Some contain decongestants or NSAIDs hidden in multi-symptom formulas.
For nausea, promethazine is commonly prescribed. It’s been used for decades and doesn’t show strong links to birth defects. But it can cause drowsiness. Natural options like ginger or vitamin B6 are often just as effective - and safer.
For heartburn, avoid bismuth subsalicylate (Pepto-Bismol) - it contains salicylates, which are related to aspirin. Loperamide (Imodium) has been linked to heart defects in one small study. H2 blockers like famotidine (Pepcid) have no solid safety data in early pregnancy, even though animal studies look fine. Stick to antacids with calcium or magnesium - they’re proven safe.
Chronic Conditions and the Risk-Benefit Balance
Some conditions can’t be ignored. Stopping your medication might be more dangerous than taking it.
If you have epilepsy, stopping your seizure meds increases the risk of fetal death by 400%. That’s not a typo. The risk of a seizure during pregnancy - and the oxygen loss it causes - is far greater than the risk from most antiepileptic drugs. The key is choosing the right one. Lamotrigine and levetiracetam have better safety profiles than valproate, which carries a high risk of neural tube defects.
If you have diabetes, uncontrolled blood sugar can raise the risk of major birth defects from 2-3% to 10-15%. That’s why tight control before and during early pregnancy is non-negotiable. Insulin is safe. Some oral diabetes pills aren’t. Talk to your doctor before you get pregnant.
Thyroid disorders like hypothyroidism need treatment too. Your body needs more thyroid hormone during pregnancy. If your TSH level stays above 2.5 mIU/L, it can affect your baby’s brain development. Levothyroxine is safe and often needs a 30-50% dose increase in the first trimester. Don’t wait for symptoms - get tested early.
Autoimmune conditions like lupus or rheumatoid arthritis? Hydroxychloroquine (Plaquenil) is safe to continue. In fact, stopping it can cause flare-ups that harm both you and your baby.
What About Acne and Antifungals?
Isotretinoin (Accutane) is one of the most dangerous drugs in pregnancy. It causes severe birth defects - including brain, heart, and facial malformations - in 20-35% of exposed pregnancies. It also carries a 30-60% risk of cognitive impairment. This isn’t a "maybe." It’s a hard no. If you’re on this drug, you must use two forms of birth control and get monthly pregnancy tests. Even a single dose can cause damage.
Antifungals like clotrimazole (topical creams for yeast infections) are safe. But oral fluconazole is a different story. One high dose (over 400 mg) early in pregnancy might increase the risk of rare birth defects. Multiple doses? Even more concern. Stick to creams and avoid pills unless your doctor says it’s absolutely necessary.
What You Can Do Right Now
You don’t need to live in fear. But you do need to be smart.
- Know your dates. Use your last period and an early ultrasound to confirm how far along you are. Timing changes everything.
- Review every medication. Prescription, OTC, herbal, supplements - write them all down. Don’t assume "natural" means safe.
- Don’t stop cold turkey. If you’re on a medication for a chronic condition, talk to your doctor before changing anything.
- Use the lowest dose for the shortest time. Even safe drugs can have risks if overused.
- Ask for alternatives. Can you manage nausea with ginger? Heartburn with diet changes? Allergies with saline rinses?
- Call MotherToBaby. They’re a free, confidential service staffed by specialists in pregnancy and medication safety. They answer over 15,000 calls a year. No judgment. Just facts.
The Big Problem: We Don’t Know Enough
Here’s the uncomfortable truth: for 96% of medications commonly used in pregnancy, there’s not enough human data to say if they’re truly safe. The FDA says 98% of prescription labels don’t give clear pregnancy risk info. That’s not because doctors are careless. It’s because pharmaceutical companies have never been required to test drugs on pregnant people.
That’s why we’re stuck with guesswork. We rely on animal studies, old case reports, and small human studies. We know acetaminophen might affect brain development. We know NSAIDs raise miscarriage risk. We know isotretinoin is devastating. But what about that new migraine med? That herbal tea? That CBD oil?
Organizations like the FDA’s Pregnancy Exposure Registry and the NIH’s PregSource project are trying to fix this. They’re collecting real-world data from thousands of pregnant people. But progress is slow. Until then, you’re your own best advocate.
Final Thought: Safety Isn’t About Avoiding Everything
It’s about making informed choices. You don’t need to suffer through nausea, headaches, or anxiety because you’re scared of pills. But you also don’t need to pop anything that makes you feel better. The goal isn’t zero risk - it’s smart risk. The goal is to protect your baby’s development while keeping you healthy enough to carry the pregnancy to term.
When in doubt, pause. Write it down. Call a specialist. Talk to your provider. You’re not being paranoid. You’re being responsible.
Is acetaminophen safe during the first trimester?
Acetaminophen is still considered the safest pain reliever during early pregnancy when used at the recommended dose (up to 4,000 mg per day). However, recent studies suggest that long-term or frequent use may be linked to a higher risk of ADHD and autism spectrum disorder in children. Use it only when necessary, at the lowest effective dose, and for the shortest time possible.
Can I take ibuprofen in the first trimester?
It’s best to avoid ibuprofen and other NSAIDs during the first trimester. Studies show they increase the risk of miscarriage by 1.6 times and may interfere with fetal heart and kidney development. Even short-term use carries risk. Stick to acetaminophen instead.
What antidepressants are safe in early pregnancy?
Sertraline and citalopram are generally considered safer options for depression during early pregnancy, with no strong link to major birth defects. Paroxetine carries a higher risk of heart defects and is usually avoided. Never stop antidepressants without talking to your doctor - untreated depression can be just as harmful to pregnancy outcomes.
Is Sudafed dangerous in the first trimester?
Pseudoephedrine (Sudafed) should be avoided in the first trimester. A 2002 study linked it to a 1.2 to 1.3 times higher risk of gastroschisis, a rare abdominal wall defect. Use saline nasal sprays, humidifiers, or steam inhalation instead for congestion.
What should I do if I took a medication before knowing I was pregnant?
Don’t panic. Most exposures don’t cause harm. The key is timing. If you took the medication before week 3, it’s likely all-or-nothing - either the embryo wasn’t affected, or it didn’t survive. After week 3, the risk depends on the drug and the exact timing. Contact MotherToBaby or your OB-GYN. They can assess your specific situation using expert databases like TERIS and give you clear, evidence-based guidance.
Are herbal supplements safe during the first trimester?
No. Just because something is "natural" doesn’t mean it’s safe. Many herbal products are unregulated and can contain harmful compounds. For example, black cohosh and dong quai can trigger contractions. High-dose vitamin A can cause birth defects. Always tell your provider about every supplement you’re taking - even if you think it’s harmless.
Can I take prenatal vitamins with other medications?
Yes, prenatal vitamins are safe and recommended. But take them separately from iron or calcium supplements, as these can interfere with absorption. Avoid high-dose vitamin A (over 10,000 IU), which can be toxic. Stick to a standard prenatal and talk to your provider before adding any extra supplements.

Steven Destiny
December 26, 2025 AT 01:32Acetaminophen is fine if you use it like a responsible adult-not like a candy. But if you’re popping Tylenol like it’s M&Ms because you’re bored, don’t act shocked when your kid needs an IEP. The science is clear: dose and duration matter. Stop the fear-mongering, start the common sense.
Fabio Raphael
December 27, 2025 AT 14:15I really appreciate how thorough this is. I’ve been on sertraline since before conception and was terrified to keep taking it-until I talked to my OB and a perinatal psychiatrist. They walked me through the data. Untreated depression carries real risks too. It’s not about avoiding meds-it’s about choosing the right ones, with support.
Sumler Luu
December 28, 2025 AT 04:41Thank you for including MotherToBaby. So many people don’t know this free service exists. I called them when I accidentally took a dose of ibuprofen before realizing I was pregnant. They calmed me down, gave me exact timing risks, and told me to just monitor. No panic. Just facts. Everyone should bookmark their site.
Sophia Daniels
December 30, 2025 AT 01:10Let’s be real-96% of meds have zero solid data because Big Pharma doesn’t want to test on pregnant people. They’d rather sell you a pill and hope you don’t miscarry. Meanwhile, your grandma took thalidomide and still had five kids. We’re not guinea pigs. We’re humans with rights to informed consent. Demand better research. Stop letting corporations decide your risk tolerance.
Peter sullen
December 31, 2025 AT 07:29It is imperative to underscore, with the utmost scientific rigor, that the embryonic period-specifically, the window of organogenesis, which spans from gestational day 17 to day 56 post-conception-is the most vulnerable phase of fetal development. Pharmacological teratogenesis is not a binary outcome; it is a dose-dependent, time-sensitive, and gene-environment-interaction-mediated phenomenon. Consequently, the utilization of acetaminophen, while currently considered the least hazardous analgesic, must be contextualized within the framework of cumulative exposure metrics, as recent longitudinal cohort analyses (e.g., CHARGE, ALSPAC) suggest potential neurodevelopmental modulation. NSAIDs, by virtue of COX-2 inhibition, may disrupt prostaglandin-mediated angiogenesis critical for cardiac and renal morphogenesis. Therefore, clinical decision-making must be predicated upon evidence-based risk-benefit stratification, not anecdotal extrapolation.
Brittany Fuhs
January 2, 2026 AT 02:22People today think they can just take whatever they want because it’s "natural" or "over the counter." My cousin took herbal tea that "helped with nausea"-turned out it had pennyroyal. Baby had brain damage. Don’t be that person. If it’s not FDA-approved for pregnancy, don’t touch it. America is falling apart because moms don’t listen to science anymore.
Nikki Brown
January 3, 2026 AT 23:14My doctor said ibuprofen was fine. I took it for 3 days. Now I’m terrified. What if I ruined my baby? 😭
Amy Lesleighter (Wales)
January 5, 2026 AT 21:35you’re not alone. i took ibuprofen too, before i knew. called mother to baby. they said 3 days? probably fine. your body knows what to do. don’t stress yourself out more than you already are. you’re doing better than you think.
Becky Baker
January 6, 2026 AT 13:24Why is everyone so scared of pills? My mom took everything in the 70s and I turned out fine. Maybe we’re just overthinking this whole thing.