G6PD Medication Safety Checker
When you have G6PD deficiency, taking the wrong medication can cause your red blood cells to break down fast-sometimes in just a day or two. This isn’t a slow, gradual problem. It’s a sudden, dangerous drop in hemoglobin that can land you in the hospital with severe anemia, dark urine, and extreme fatigue. The good news? Almost all of these cases are preventable. You don’t need to avoid every drug. You just need to know which ones are risky and how to protect yourself.
What Exactly Is G6PD Deficiency?
G6PD stands for Glucose-6-Phosphate Dehydrogenase. It’s an enzyme your red blood cells use to fight off oxidative stress. Think of it like a shield. When you take certain drugs, smoke, eat fava beans, or get an infection, your body produces free radicals-harmful molecules that can damage your red blood cells. G6PD helps neutralize them. If you’re deficient, your shield is weak. Without it, those cells burst open, spilling hemoglobin into your bloodstream. That’s hemolysis.
This isn’t rare. Around 400 million people worldwide have it. In places like sub-Saharan Africa, the Mediterranean, and Southeast Asia, up to 1 in 5 people carry a version of the gene. It’s more common in men because it’s linked to the X chromosome, but women can be affected too-about 15% of female carriers experience symptoms due to how X-chromosome inactivation works. Many people live their whole lives without knowing they have it… until they take a medication that triggers a crisis.
Which Medications Are Dangerous?
The World Health Organization lists 87 medications that can cause hemolysis in people with G6PD deficiency. Not all are equally risky, but some are absolute no-go zones.
- Rasburicase-used to treat tumor lysis syndrome. It causes 100% hemolysis in deficient patients. The FDA issued a Black Box Warning in January 2023. Never give this without testing first.
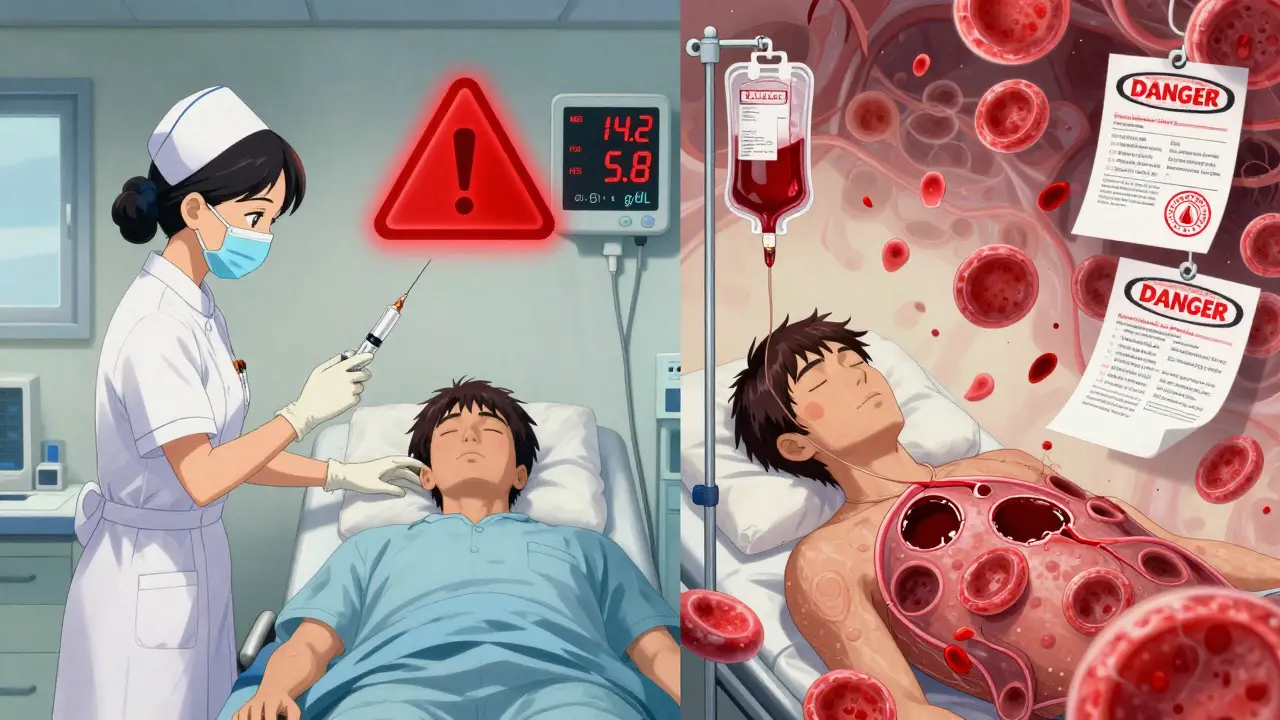
- Methylene blue-used for methemoglobinemia. In G6PD-deficient people, it causes severe hemolysis in 95% of cases. A 2021 JAMA case series showed a patient’s hemoglobin dropped from 14.2 to 5.8 g/dL in 48 hours after receiving it.
- Primaquine-a malaria drug. Standard doses cause hemolysis in 100% of people with Class I or II deficiency. WHO updated its guidelines in 2023 to require G6PD testing before use.
- Dapsone-used for leprosy and some skin conditions. Hemolysis occurs in 80% of deficient patients at doses above 50 mg daily.
- Sulfonamides-like sulfamethoxazole (Bactrim). Risk is lower than the above, but still real. Avoid if you’ve had prior reactions.
Some drugs have mixed evidence. Sulfonylureas like glyburide (used for diabetes) carry warnings on 92% of labels, but only 17 documented cases exist since 1965. Still, many doctors err on the side of caution. Always check.
What Medications Are Safe?
You don’t have to live in fear. Many common medications are completely safe.
- Chloroquine-safe for malaria prevention in all G6PD deficiency classes.
- Tafenoquine-a newer malaria drug approved in 2018. Safe-but only if you’ve been tested and cleared. It requires mandatory screening.
- Artemisinin-based combination therapies-the gold standard for malaria treatment. No risk of hemolysis.
- Atovaquone-proguanil (Malarone)-a safe alternative for travelers to malaria zones.
- Most antibiotics-penicillin, amoxicillin, ciprofloxacin, and azithromycin are all safe.
- Common painkillers-acetaminophen and ibuprofen are fine at normal doses.
The key is knowing your variant. People with the G6PD A- variant (common in Africa) tend to have milder reactions than those with the Mediterranean variant (common in Southern Europe). But since you can’t always know your variant without genetic testing, it’s safest to assume you’re at risk and avoid the known triggers.
Why Testing Matters-And When to Get It
Testing is the only way to know for sure. But timing matters. If you’ve had a recent hemolytic episode, your enzyme levels may look normal because your body is making new red blood cells. That’s misleading. Wait at least 3 months after a crisis before testing.
The best test is a quantitative spectrophotometric assay, which measures enzyme activity in units per gram of hemoglobin. Deficiency is defined as:
- Class I: Less than 10% of normal (under 1.7 U/g Hb)
- Class II: 1-10% (1.7-4.5 U/g Hb)
- Class III: 10-60% (4.5-12.0 U/g Hb)
Point-of-care tests are now available. The STANDARD G6PD Test System, approved by the FDA in January 2024, gives results in 8 minutes with 99.1% accuracy. It’s being rolled out in emergency rooms and clinics in malaria-endemic regions.
Many countries now screen newborns. Saudi Arabia reduced hemolytic crisis admissions by 78% after implementing universal screening. In the U.S., only 12 states require it-even though 1 in 10 African American males has G6PD deficiency. If you’re from a high-prevalence region, ask for testing. Don’t wait for a crisis.
Real-World Consequences of Skipping Testing
Stories from the front lines show how easily this can go wrong.
In one case, a 28-year-old man with tumor lysis syndrome was given rasburicase without G6PD testing. His hemoglobin crashed to 3.1 g/dL. He needed 10 units of blood over three days. He survived-but barely.
A nurse on Reddit shared how she gave methylene blue to a patient who hadn’t been tested. The patient’s hemoglobin dropped from 14.2 to 5.8 in under two days. Three units of blood transfusions later, he was stable.
On the flip side, a hospital in Thailand implemented mandatory G6PD testing before giving primaquine to malaria patients. In four years, hemolytic crises dropped from 15.2% to 0.3%. That’s not luck. That’s protocol.
Patients who get proper education are far less likely to have problems. A 2023 NIH study found that 92% of G6PD-deficient patients who received clear avoidance guidance had no hemolytic episodes over five years. Only 38% of those who didn’t get education stayed crisis-free.

What You Can Do Right Now
If you’ve never been tested and you’re from a high-risk region (Africa, Mediterranean, Southeast Asia), get tested. It’s simple. A finger prick. Results in minutes.
If you’ve been diagnosed:
- Carry a medical alert card or bracelet that says “G6PD Deficiency.”
- Keep a list of safe and unsafe medications. Update it every time you see a new doctor.
- Ask every prescriber: “Is this safe for someone with G6PD deficiency?” Don’t assume they know.
- For malaria prevention, use Malarone instead of primaquine.
- Avoid fava beans and naphthalene (mothballs). These can also trigger hemolysis.
- If you feel sudden fatigue, dark urine, or jaundice after starting a new drug, stop it and seek help immediately.
The Bigger Picture: Progress and Gaps
The global market for G6PD testing is growing fast-projected to hit $313 million by 2028. The WHO, FDA, and Global Fund are pushing for universal screening in malaria-endemic countries. The Global Fund has pledged $127 million to build testing infrastructure in 32 countries.
But progress is uneven. Only 18 of 47 African countries have national screening programs. In the U.S., most hospitals still don’t test unless there’s a family history or obvious risk. Many doctors still think only men are affected. They’re wrong.
Research is moving forward. A 2024 study showed that N-acetylcysteine (NAC) may protect red blood cells from oxidative damage when taken with risky drugs. Phase I trials for enzyme replacement therapy begin in late 2024. The goal? Make G6PD deficiency no longer a death sentence.
Until then, prevention is everything. A simple test. A few questions. A list of safe drugs. That’s all it takes to avoid a life-threatening crisis.
What to Do If You’ve Already Had a Hemolytic Episode
If you’ve had one, you’re at higher risk for another. Here’s what to do:
- Wait at least 3 months before getting tested. Your new red blood cells will have normal enzyme levels, giving a false sense of security.
- Document every drug you took before the episode. Share this with your hematologist.
- Ask for a genetic test to identify your variant. This helps tailor your risk profile.
- Register with a G6PD registry if one exists in your country. It helps track outcomes and improve guidelines.
Can women have G6PD deficiency too?
Yes. While the gene is on the X chromosome and more common in men, women can be affected. About 15% of female carriers experience hemolysis due to random X-chromosome inactivation. This means some of their red blood cells lack the enzyme, while others don’t. If enough are deficient, they can still have a hemolytic crisis. Never assume women are safe just because they’re not male.
Is G6PD deficiency the same as sickle cell?
No. Sickle cell is a structural problem with hemoglobin that causes cells to deform and block blood flow. G6PD deficiency is a metabolic problem-your red blood cells can’t defend against oxidative stress. Both can cause anemia, but the triggers, treatments, and long-term risks are completely different. Splenectomy helps sickle cell patients but does nothing for G6PD deficiency.
Can I take antibiotics if I have G6PD deficiency?
Most are safe. Penicillin, amoxicillin, azithromycin, ciprofloxacin, and doxycycline are all considered safe. Avoid sulfonamides like Bactrim unless you’ve been cleared by your doctor. Always double-check with a pharmacist or hematologist if you’re unsure.
What should I do if I accidentally take a risky drug?
Stop the drug immediately. Drink plenty of fluids. Go to the emergency room if you notice dark urine, yellowing skin, extreme fatigue, or rapid heartbeat. Hemolysis can progress quickly. Early intervention-like IV fluids and blood transfusions-can prevent kidney damage and death.
Are there any new treatments on the horizon?
Yes. Research is advancing on two fronts. First, N-acetylcysteine (NAC) shows promise in protecting red blood cells from oxidative damage when taken alongside risky drugs. Second, Phase I trials for recombinant human G6PD enzyme replacement therapy are scheduled to begin in late 2024. These could eventually allow people to receive the missing enzyme directly, preventing hemolysis before it starts.

