By the end of 2024, more than 300 drugs were in short supply across the United States. Cancer treatments, antibiotics, anesthetics, and even basic saline solutions became harder to find in hospitals. This wasn’t a one-time crisis-it’s the new normal. And the federal government is finally trying to fix it. But the solutions being pushed right now are uneven, underfunded, and missing the real problem.
What’s Actually Being Stockpiled-and Why It’s Not Enough
In August 2025, President Trump signed Executive Order 14178, expanding the Strategic Active Pharmaceutical Ingredients Reserve (SAPIR). This program doesn’t stockpile pills or injections. It stores the raw chemical building blocks-active pharmaceutical ingredients (APIs)-needed to make 26 critical drugs. The idea is simple: APIs last longer, cost less to store, and are easier to ship than finished medicines. They’re also harder for foreign suppliers to hold hostage. The FDA says China supplies about 80% of the APIs used in U.S. medications. That’s a huge risk. If a factory in Shanghai shuts down, or a shipping lane gets blocked, hospitals feel it months later. SAPIR aims to cut that dependency by keeping enough raw material on hand to produce these drugs domestically during emergencies. But here’s the catch: only 26 drugs are covered. That’s less than 5% of all medications that have ever gone short. The FDA’s own database shows over 1,200 drugs have faced shortages since 2012. Oncology drugs alone made up 31% of all shortages in 2024, yet only 4% of SAPIR’s list focuses on them. A hospital treating a leukemia patient might find their chemo drug gone, but the federal reserve won’t help because it’s not on the list.The FDA’s Role: Fixing Problems, Not Preventing Them
The FDA doesn’t just sit back and watch shortages happen. They work directly with manufacturers to fix them. In 85% of cases, they help by speeding up inspections, letting in temporary imports, or approving new production lines. That’s how they resolved the 2018-2020 saline shortage that hit 90% of U.S. hospitals. But prevention? That’s where things fall apart. Federal law requires drugmakers to report potential shortages six months in advance. In theory, that gives the system time to react. In practice? Only 58% of companies report on time. Small manufacturers-those with fewer than 50 employees-are even worse, missing reporting deadlines 82% of the time. The FDA’s new AI-powered monitoring system, launched in November 2025, tries to fill that gap. It tracks shipping data, hospital orders, and factory output across 17 sources to predict shortages 90 days ahead with 82% accuracy. That’s impressive. But if manufacturers aren’t telling the FDA what’s going wrong, even the smartest algorithm is flying blind. And enforcement? Nearly nonexistent. Between 2020 and 2024, the FDA issued just 17 warning letters for failure to report shortages. In the European Union, under similar rules, they issued 142. No penalties. No consequences. Why would a company risk losing money by reporting a problem early?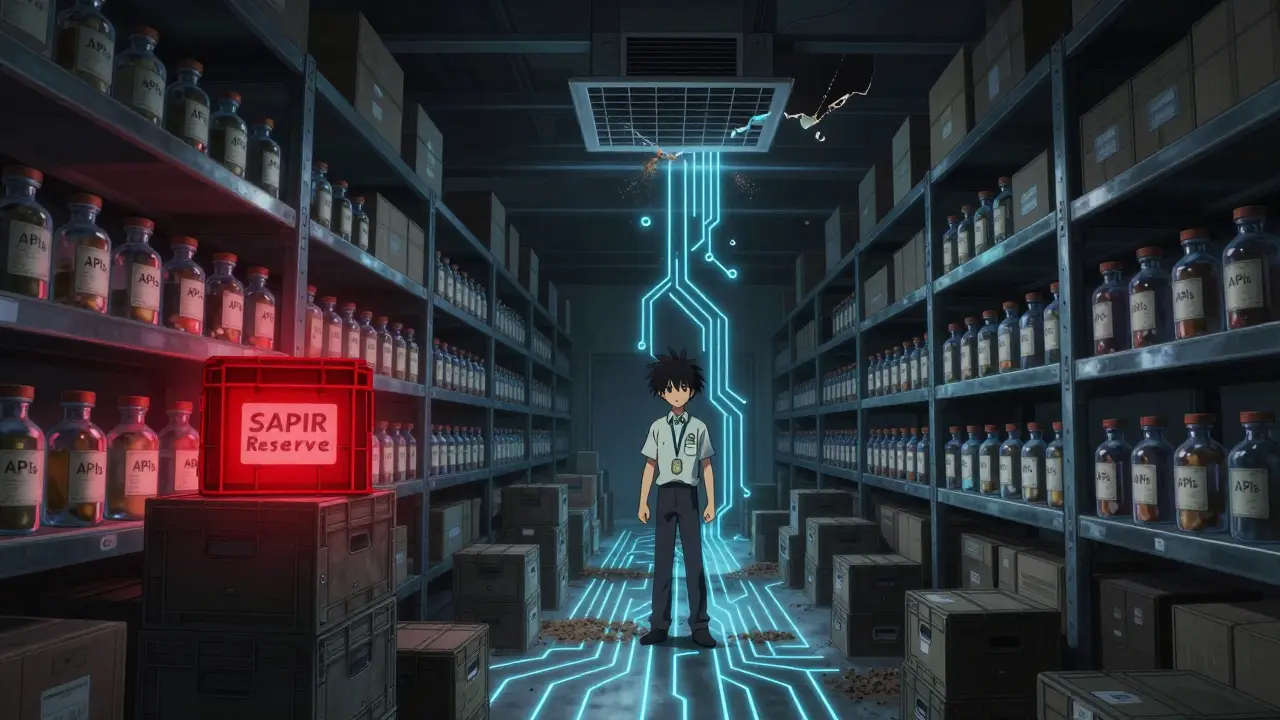
Why Domestic Manufacturing Isn’t Coming Back
The government keeps talking about bringing drug production back to the U.S. But the numbers don’t lie. In 2024, the FDA approved 56 new manufacturing facilities for critical drugs. Of those, 42% were built in Ireland and Singapore-not America. Why? Because it’s cheaper and faster overseas. Building a new API plant in the U.S. takes 28 to 36 months just to get FDA approval. In the EU, it’s 18 to 24 months. That’s a two-year delay just to get started. Then there’s the money problem. Sterile injectables-like antibiotics and painkillers-make up 73% of all shortages. They’re cheap to make, and the profit margins are razor-thin. No company wants to invest millions in a factory that might only earn $0.50 per dose. The market doesn’t reward safety or redundancy. It rewards low cost. The Department of Commerce announced $285 million in CHIPS Act funding for pharmaceutical plants in September 2025. Sounds big. But industry analysts say it covers less than 5% of the $6 billion needed to build enough domestic capacity to make a real difference.What’s Working? The One Thing Everyone Agrees On
There’s one federal program that actually works: the FDA’s Early Notification Pilot Program. Hospitals and pharmacies that join this program report shortages faster and get better support. The result? Shortages last 28% less time. Why? Because it gives them tools, training, and direct access to FDA experts. It turns hospitals from passive victims into active partners. But here’s the irony: the current administration has weakened this program’s requirements. Mandatory reporting? Reduced. Funding? Cut. Support staff? Gone. Meanwhile, the European Union has a centralized system where every member state shares real-time data on drug availability. Between 2022 and 2024, that system cut shortages by 37%. The U.S. could do the same. But it would require cooperation, funding, and political will-all things that are in short supply.


Angel Tiestos lopez
January 13, 2026 AT 13:52Alan Lin
January 14, 2026 AT 21:07Priyanka Kumari
January 15, 2026 AT 20:09Avneet Singh
January 17, 2026 AT 18:38Nelly Oruko
January 18, 2026 AT 05:46vishnu priyanka
January 18, 2026 AT 20:53Lethabo Phalafala
January 20, 2026 AT 20:33Lance Nickie
January 21, 2026 AT 23:32Milla Masliy
January 23, 2026 AT 20:50Damario Brown
January 25, 2026 AT 11:09sam abas
January 26, 2026 AT 06:42