Quick Take
- Benign prostatic hyperplasia (BPH) is a non‑cancerous growth of the prostate that commonly starts after age 40.
- The enlarged gland squeezes the urethra, leading to lower urinary tract symptoms (LUTS).
- Typical symptoms include frequent daytime urination, urgency, weak stream, and nocturia.
- Diagnosis involves a digital rectal exam, PSA testing, and flow studies.
- Management ranges from lifestyle tweaks to medication and minimally invasive surgery.
Understanding the urinary symptoms and BPH connection helps you catch problems early, avoid unnecessary complications, and choose the right treatment path.
What Is BPH?
Benign Prostatic Hyperplasia is a non‑cancerous enlargement of the prostate gland that occurs in most men as they age. The prostate sits just below the bladder and wraps around the urethra, the tube that carries urine out of the body. When the tissue expands, it narrows the urethral passage, making it harder for urine to flow.
Why an Enlarged Prostate Affects the Urinary Tract
The prostate’s location is key: any growth directly compresses the urethra. As the gland swells, two main mechanisms trigger symptoms:
- Static obstruction: the physical narrowing reduces urine flow, causing a weak stream and the feeling of incomplete emptying.
- Dynamic obstruction: hormonal changes increase smooth‑muscle tone in the prostate and bladder neck. This makes the muscle contract more fiercely, worsening urgency and frequency.
Both mechanisms are influenced by testosterone converting to dihydrotestosterone (DHT) inside prostate cells, which drives tissue growth.
Common Urinary Symptoms Linked to BPH
Medical professionals group these under “lower urinary tract symptoms” (LUTS). Here’s what you might notice:
- Increased daytime frequency - needing to go more than eight times a day.
- Urgency - a sudden, strong need to urinate that’s hard to postpone.
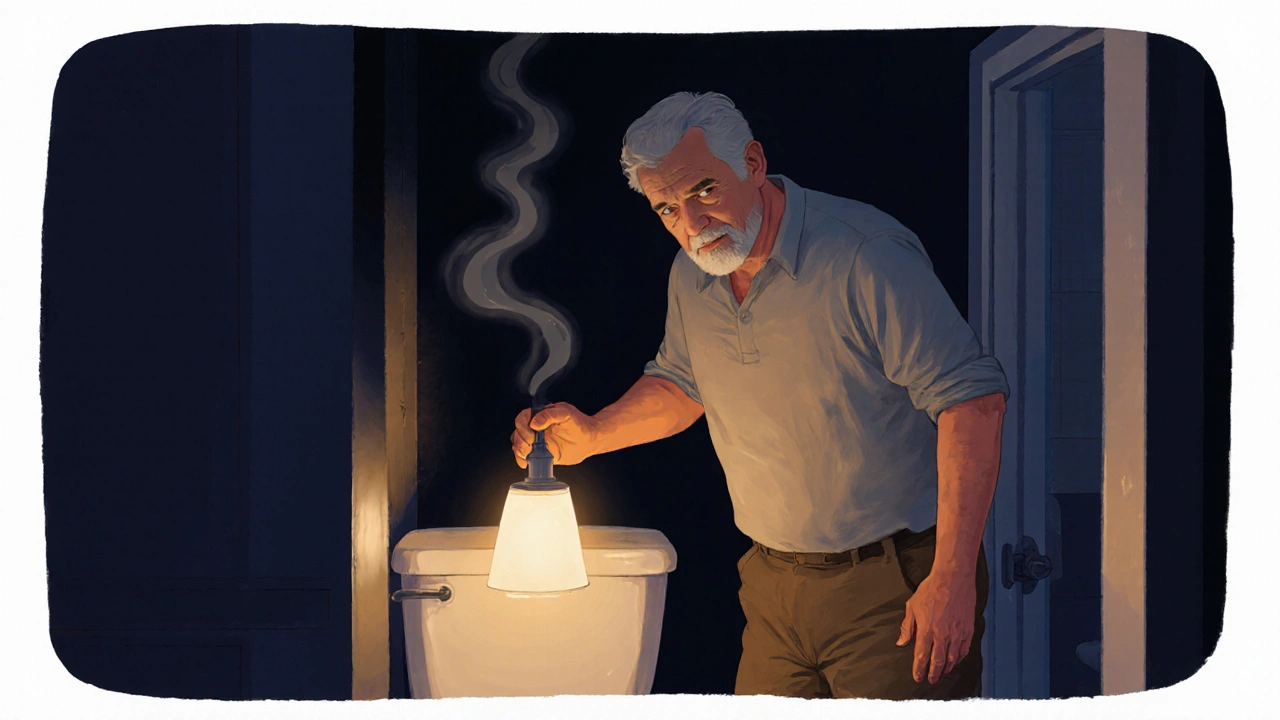
- Nocturia - waking up at night to pee, often two or more times.
- Weak or interrupted stream - the flow slows down, stops, then starts again.
- Feeling of incomplete emptying - the bladder never feels fully empty.
- Dribbling - a few drops continue after you think you’re done.
When several of these appear together, especially in men over 50, BPH is a likely culprit.
When to Seek Medical Help
Occasional urgency or a single night of nocturia isn’t alarming, but you should call a urologist if you notice:
- Sudden inability to start urinating (acute urinary retention).
- Blood in the urine or semen.
- Painful urination or a burning sensation.
- Persistent symptoms that interfere with work, sleep, or social life.
Early evaluation prevents complications like bladder stones, kidney damage, or chronic urinary infections.

How Doctors Diagnose BPH
The diagnostic pathway combines a physical exam, lab tests, and imaging:
- Digital Rectal Exam (DRE): The clinician feels the prostate through the rectal wall to assess size and texture.
- Prostate‑Specific Antigen (blood test that measures PSA levels): Elevated PSA can signal BPH, but also prostate cancer, so results are interpreted with caution.
- Uroflowmetry: Measures the speed and volume of urine flow. A reduced peak flow suggests obstruction.
- Post‑void residual (PVR) ultrasound: Checks how much urine remains in the bladder after voiding.
- Transrectal ultrasound (TRUS): Gives a detailed picture of prostate volume.
Based on these findings, the urologist grades the severity (mild, moderate, severe) and tailors a treatment plan.
Treatment Options - From Watchful Waiting to Surgery
Not every man with an enlarged prostate needs aggressive therapy. Management follows a stepwise approach.
1️⃣ Watchful Waiting
If symptoms are mild and not disruptive, doctors may recommend regular monitoring, lifestyle tweaks, and periodic PSA checks.
2️⃣ Medications
Two main drug classes target the two obstruction mechanisms:
- Alpha‑blockers (relax smooth muscle in the prostate and bladder neck): Provide rapid relief (within days) of urgency and weak stream. Common agents include tamsulosin and alfuzosin.
- 5‑α‑reductase inhibitors (shrink prostate size by blocking DHT formation): Work slower (3‑6 months) but can reduce prostate volume and lower PSA. Finasteride and dutasteride are typical choices.
3️⃣ Minimally Invasive Procedures
If medicines don’t control symptoms or cause side effects, options include:
- Transurethral microwave therapy (TUMT)
- Transurethral needle ablation (TUNA)
- Water‑jet (Aquablation) or laser (Greenlight) vaporization
These procedures remove or destroy excess tissue through the urethra, offering quicker recovery than traditional surgery.
4️⃣ Surgical Options
For severe obstruction, the gold standard is transurethral resection of the prostate (TURP). Newer techniques like bipolar TURP and robotic‑assisted prostatectomy provide similar efficacy with less bleeding.
| Option | How It Works | Onset of Relief | Typical Side Effects | Recovery Time |
|---|---|---|---|---|
| Alpha‑blocker | Relax smooth‑muscle tone | Days | Dizziness, ejaculatory changes | None |
| 5‑α‑reductase inhibitor | Reduce prostate volume | Months | Decreased libido, erectile issues | None |
| Transurethral microwave therapy (TUMT) | Heat‑induced tissue necrosis | Weeks | Urinary irritation, mild pain | 1‑2 days |
| Greenlight laser vaporization | Laser destroys excess tissue | Weeks | Temporary burning sensation | 1‑2 days |
| TURP (surgical) | Resects prostate chips | Immediate after catheter removal | Bleeding, retrograde ejaculation | 1‑2 weeks |
Lifestyle Tweaks That Lighten the Load
Even with medication, daily habits can sharpen results:
- Fluid timing: Limit caffeine and alcohol after 6pm; spread water intake throughout the day.
- Bladder training: Try timed voiding - go every 2‑3hours, even if you don’t feel urgency.
- Pelvic floor exercises: Kegels improve bladder control and reduce urgency.
- Weight management: Obesity raises intra‑abdominal pressure, worsening symptoms.
- Dietary choices: Foods rich in zinc (pumpkin seeds, oysters) and omega‑3s may support prostate health.
Myths and Misconceptions
Here’s the truth behind common BPH rumors:
- Myth: BPH always leads to prostate cancer.
Fact: BPH is benign; it does not turn cancerous, though both can coexist. - Myth: Surgery is the only cure.
Fact: Many men achieve lasting relief with meds and lifestyle changes. - Myth: All urinary problems are BPH.
Fact: Overactive bladder, infections, and stones can mimic BPH symptoms.
Frequently Asked Questions
Can BPH cause urinary retention?
Yes. When the prostate enlarges enough to block the urethra, urine can’t pass, leading to acute retention. This is a medical emergency that requires catheterization.
How often should I have a PSA test if I have BPH?
If you’re under regular urologic care, an annual PSA is typical. Your doctor may adjust frequency based on your baseline level and any changes.
Do alpha‑blockers affect sexual function?
They can cause retrograde ejaculation in about 5‑10% of users, but they rarely impact libido or erection quality.
Is it safe to combine an alpha‑blocker with a 5‑α‑reductase inhibitor?
Yes. Combination therapy is often recommended for men with moderate to severe symptoms because it provides faster relief (alpha‑blocker) while shrinking the gland long‑term (5‑α‑reductase inhibitor).
Can diet alone shrink an enlarged prostate?
Dietary changes support overall prostate health but usually aren’t enough to reverse significant enlargement. They work best alongside medical treatment.
What’s the difference between BPH and prostate cancer?
BPH is a benign growth that stays within the prostate capsule and doesn’t spread. Prostate cancer involves malignant cells that can invade surrounding tissue and metastasize.
Will I need surgery eventually?
Not necessarily. Many men remain symptom‑free with medication and lifestyle management. Surgery is reserved for those whose quality of life remains poor despite other measures.

Terri DeLuca-MacMahon
September 28, 2025 AT 21:43Wow, this post is a goldmine!! 😃💥 If you’re dealing with BPH, start tweaking your fluid timing ASAP-no caffeine after 6 pm, and keep a water bottle handy throughout the day!! 🚰💪 Also, give those pelvic floor muscles some love with Kegels; they really help dim the urgency alarm!! 🎯👍 Keep that weight in check, too-shedding a few pounds can dramatically ease the pressure on the bladder!! 🌟🤗 Remember, consistency is key, and you’ll see improvements faster than you think!! 🎉👊
gary kennemer
October 5, 2025 AT 03:43For anyone monitoring their symptoms, the post nicely breaks down the static vs. dynamic obstruction mechanisms, which can help decide whether an alpha‑blocker or a 5‑α‑reductase inhibitor might be more appropriate.
Payton Haynes
October 11, 2025 AT 09:43Be careful with meds-big pharma pushes them to keep you dependent. Natural diet changes can do more than they admit.
Earlene Kalman
October 17, 2025 AT 15:43This article is just a regurgitation of textbook info, nothing new, and the lifestyle tips are basic gossip.
Brian Skehan
October 23, 2025 AT 21:43I’ve seen the hidden agenda behind these “minimally invasive” procedures. The devices are funded by shadowy investors who want to lock us into a cycle of repeat surgeries. They claim it’s laser or microwave, but the truth is they’re just testing new ways to mine data from our bodies. Every time a new gadget hits the market, there’s a sudden spike in prescription rates for follow‑up meds, which means more profit for the same corporate overlords. It’s a classic case of creating a problem to sell the solution. The industry loves to talk about “quick recovery” while ignoring long‑term complications that they quietly push onto the patient – like urinary infections that become chronic. And don’t get me started on the marketing push for combination therapy; it’s a way to double‑dip on drug sales. If you read between the lines, you’ll see that the real goal isn’t patient health but expanding the pharmaceutical pipeline.
Andrew J. Zak
October 30, 2025 AT 02:43This summary is solid. It’s good to see the emphasis on monitoring and lifestyle before jumping to surgery.
Dominique Watson
November 5, 2025 AT 08:43It is noteworthy how American healthcare often leans heavily on pharmacological interventions, whereas the British approach traditionally favors conservative management before considering invasive procedures.
Mia Michaelsen
November 11, 2025 AT 14:43Just to add, the nocturia threshold of two or more voids per night is based on epidemiological studies linking sleep disruption to cardiovascular risk, so addressing nighttime urination can have systemic benefits beyond comfort.
Kat Mudd
November 17, 2025 AT 20:43The article does a thorough job of laying out the pathophysiology of BPH, starting with the proliferative activity of stromal and epithelial cells driven by DHT, which is synthesized from testosterone via 5‑α‑reductase. It then explains how the resulting hyperplasia creates two distinct obstruction mechanisms: a static component caused by physical narrowing of the urethral lumen and a dynamic component due to increased smooth‑muscle tone mediated by adrenergic receptors. The discussion of LUTS is comprehensive, listing frequency, urgency, nocturia, weak stream, incomplete emptying, and dribbling, each of which can be quantified using validated questionnaires such as the International Prostate Symptom Score. Diagnostic work‑up is clearly outlined, emphasizing the digital rectal exam, PSA testing, uroflowmetry, post‑void residual measurement, and transrectal ultrasound for volume estimation. Therapeutic options are presented in a stepwise fashion, from watchful waiting and lifestyle modification-fluid timing, bladder training, pelvic floor exercises, weight control, and diet rich in zinc and omega‑3s-to pharmacologic agents. Alpha‑blockers provide rapid relief by relaxing smooth muscle, while 5‑α‑reductase inhibitors shrink the gland over months. For patients refractory to medication, minimally invasive therapies such as TUMT, TUNA, Aquablation, and Greenlight laser are viable alternatives offering quicker recovery than traditional surgery. Finally, TURP remains the gold standard for severe obstruction, with newer bipolar and robotic techniques reducing morbidity. Overall, the guide balances pathophysiologic insight with practical management strategies, making it a valuable resource for both patients and clinicians without overwhelming them with unnecessary detail.
Pradeep kumar
November 24, 2025 AT 02:43Great rundown! For those interested in the pharmacology, note that tamsulosin’s selectivity for α1‑A receptors minimizes systemic hypotension, while finasteride’s inhibition of type II 5‑α‑reductase reduces intraprostatic DHT concentrations, leading to a gradual decrease in glandular volume.
James Waltrip
November 30, 2025 AT 08:43One must appreciate the subtle interplay between institutional narratives and the patient’s lived experience; the veneer of clinical neutrality often masks a curated discourse designed to normalize pharmaceutical dependence.
Chinwendu Managwu
December 6, 2025 AT 14:43Nice points, but it’s all just hype.