Tetracycline is a broad‑spectrum antibiotic that inhibits bacterial protein synthesis by binding to the 30S ribosomal subunit. First isolated in the 1940s, it remains on the WHO Essential Medicines List and is frequently prescribed for skin infections such as acne, impetigo, and cellulitis.
When a rash, boil, or pustule won’t clear up, many clinicians reach for tetracycline because it’s cheap, oral, and effective against a wide range of Gram‑positive and Gram‑negative bacteria. Yet the drug isn’t a magic bullet - proper dosing, awareness of side effects, and vigilance about resistance are essential for success.
How Tetracycline Works on the Skin
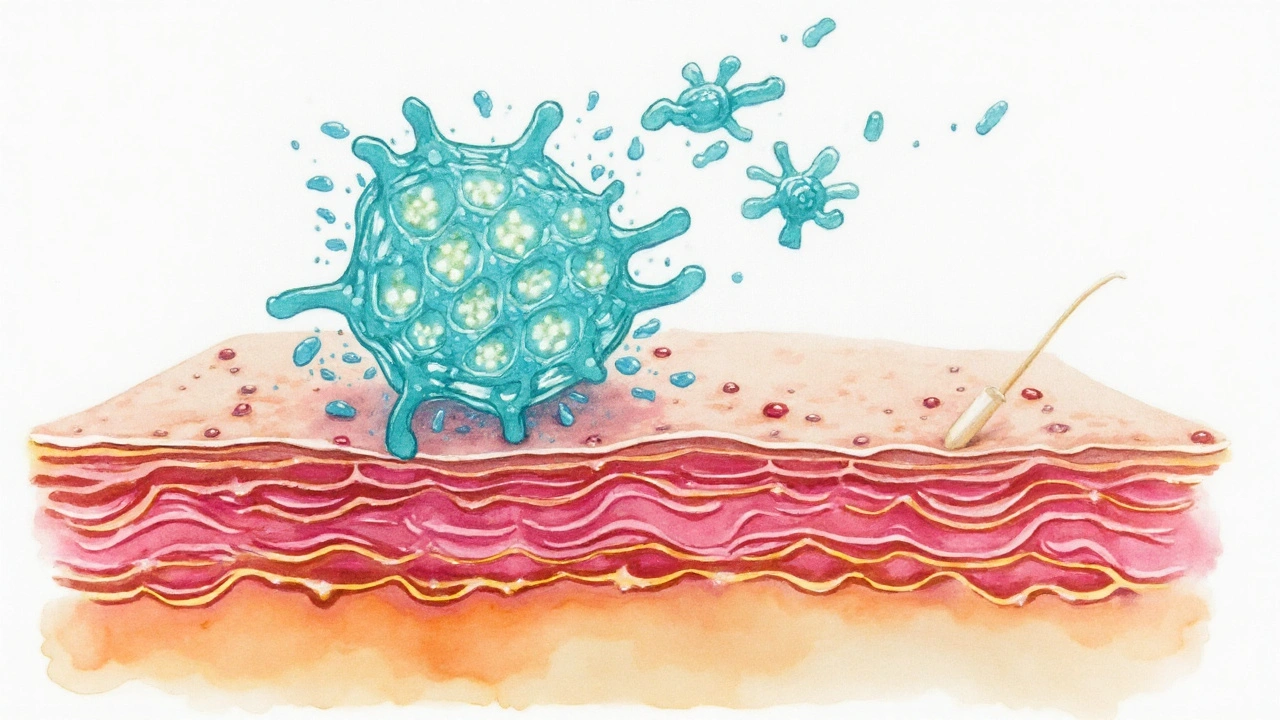
Once absorbed, tetracycline circulates into the dermis and epidermis, where it blocks the addition of new amino acids to bacterial proteins. This bacteriostatic action stalls the growth of organisms like Staphylococcus aureus, a common cause of cellulitis and impetigo. For acne, the drug also reduces inflammation by dampening the activity of neutrophils and decreasing the production of inflammatory cytokines.
When to Use Tetracycline for Skin Infections
Typical indications include:
- Uncomplicated acne vulgaris (moderate‑to‑severe inflammatory lesions)
- Impetigo caused by Staphylococcus aureus or Streptococcus pyogenes
- Early‑stage cellulitis when oral therapy is appropriate
- Folliculitis and other superficial follicular infections
For deep tissue infections, hospitals often prefer intravenous agents, but for most outpatient skin conditions, oral tetracycline is a first‑line option.
Dosage and Administration
Adults usually receive 250-500mg every 6-12hours, depending on severity. Children under 8years are generally excluded because of permanent tooth discoloration. A typical regimen looks like this:
- Take the first dose with a full glass of water.
- Repeat every 8hours for 7-14days.
- Avoid dairy, calcium supplements, and antacids within two hours of dosing-these bind the drug and cut absorption by up to 50%.
Therapeutic drug monitoring isn’t routine, but for patients with renal failure, the dose may be reduced to 250mg twice daily.
Safety Profile: Side Effects and Contra‑indications
Most people tolerate tetracycline well, but be on the lookout for:
- Gastrointestinal upset (nausea, vomiting, diarrhea)
- Photosensitivity - patients should use sunscreen and wear protective clothing outdoors.
- Tooth discoloration and enamel hypoplasia in children < 8years.
- Rare hepatotoxicity and intracranial hypertension (especially in women of child‑bearing age).
Contra‑indications include pregnancy (Category D), known hypersensitivity, and severe liver disease. If a patient reports persistent nausea or a skin rash, switch to an alternative like Doxycycline or Clindamycin.
Resistance: Why It Matters
Over the past two decades, tetracycline‑resistant strains of MRSA (methicillin‑resistant Staphylococcus aureus) have risen, especially in community settings. Resistance mechanisms include efflux pumps and ribosomal protection proteins. To preserve efficacy:
- Reserve tetracycline for confirmed susceptible organisms.
- Complete the full course - stopping early fuels resistance.
- Combine with topical agents (e.g., benzoyl peroxide for acne) to reduce bacterial load.
National guidelines, such as those from the FDA, advise culture‑guided therapy when possible.
Comparison with Other Oral Antibiotics
| Attribute | Tetracycline | Doxycycline | Clindamycin |
|---|---|---|---|
| Spectrum | Broad (Gram‑+, Gram‑‑, atypicals) | Broad, stronger against anaerobes | Excellent for Gram‑+ anaerobes, MRSA |
| Typical oral dose | 250-500mg q6‑12h | 100mg q12h | 300mg q6h |
| Common side effects | Photosensitivity, GI upset | Less photosensitivity, GI upset | Diarrhea, C.difficile risk |
| Pregnancy safety | Category D (avoid) | Category B (more acceptable) | Category B |
| Resistance concern | Increasing tetracycline‑resistance | Lower resistance rates | High MRSA resistance in some regions |
For most healthy adults with mild‑to‑moderate acne, tetracycline skin infection therapy is cost‑effective. In pregnant patients or those with severe photosensitivity, doxycycline may be a safer choice, while clindamycin shines against resistant Gram‑positive organisms.
Practical Tips for Clinicians and Patients
- Check susceptibility. Lab tests confirming Staphylococcus aureus sensitivity guide whether tetracycline will work.
- Educate on food interactions. Dairy and calcium supplements are the biggest absorptive roadblocks.
- Monitor liver function. Baseline AST/ALT in patients with known hepatic disease.
- Use sunscreen. Recommend SPF30+ and protective clothing for patients on therapy.
- Document outcome. Record lesion size reduction and any adverse events at day7 and day14.
Following these steps keeps the treatment safe, effective, and minimizes the chance of developing resistant strains.
Related Concepts and Next Steps
Understanding tetracycline fits into a broader picture of antibiotic stewardship. Good stewardship means prescribing the narrowest effective agent, using the shortest effective duration, and educating patients about adherence. Readers interested in the big picture may explore topics such as:
- Mechanisms of bacterial resistance (efflux pumps, ribosomal protection)
- Topical versus oral therapy for acne
- Guidelines from the WHO Essential Medicines List on skin infection management
- Emerging oral agents like omadacycline
Each of these areas builds on the foundation covered here and can help clinicians stay ahead of evolving resistance patterns.

Frequently Asked Questions
Can I take tetracycline if I’m pregnant?
No. Tetracycline is classified as Pregnancy Category D because it can cause tooth discoloration and inhibit bone growth in the fetus. Safer alternatives like doxycycline or clindamycin are preferred.
How long should I stay on tetracycline for acne?
Typical courses last 8‑12weeks. Some dermatologists extend therapy up to 6months if lesions keep improving, but treatment should be reassessed after the initial 2‑month period.
Why does tetracycline cause photosensitivity?
The drug accumulates in the skin and, when exposed to UV light, generates reactive oxygen species that damage skin cells. This reaction explains the heightened sunburn risk.
Is it safe to take tetracycline with calcium supplements?
No. Calcium chelates tetracycline, dropping its absorption by up to 50%. Space the supplement at least two hours before or after the antibiotic.
What should I do if I develop a rash while on tetracycline?
Stop the medication immediately and contact your healthcare provider. A rash could signal an allergic reaction or a severe side effect like Stevens‑Johnson syndrome, which requires urgent evaluation.
How does tetracycline compare to doxycycline for treating skin infections?
Both belong to the tetracycline class, but doxycycline has a longer half‑life, allowing twice‑daily dosing, and causes less photosensitivity. Doxycycline also has a slightly better resistance profile. However, both are effective; choice often hinges on patient tolerance and cost.
Can children under 8 years take tetracycline?
No. The drug can permanently stain developing teeth and affect bone growth. For pediatric skin infections, other antibiotics like amoxicillin or cephalexin are recommended.


Darrell Wardsteele
September 22, 2025 AT 00:34Tetracycline still works if you dont screw up the dose.
Madeline Leech
September 28, 2025 AT 17:30Pregnancy is a non‑negotiable red flag – tetracycline belongs in Category D and you should never prescribe it to a pregnant patient. The drug’s propensity to cause permanent tooth discoloration in the fetus makes any cost savings irrelevant. Doctors who ignore this are putting future generations at risk for avoidable dental problems. It’s not just a guideline; it’s an ethical duty to protect unborn children.
Barry White Jr
October 5, 2025 AT 10:27Totally agree – safety first and the risks just aren’t worth it.
Andrea Rivarola
October 12, 2025 AT 03:23Tetracycline remains a workhorse in dermatology, but its success hinges on proper patient counseling.
Before starting therapy, clinicians should verify that the patient has no history of photosensitivity or recent sun exposure.
Explaining the importance of sunscreen with an SPF of at least 30 can prevent painful burns that might otherwise be blamed on the medication.
Dietary advice is equally critical; patients must understand that dairy products and calcium supplements can chelate the drug and halve its absorption.
A simple rule of thumb is to take the pill with a full glass of water and wait at least two hours before consuming any calcium‑rich foods.
Monitoring liver enzymes at baseline is prudent for anyone with known hepatic impairment, as tetracycline is partially metabolized hepatically.
For patients with reduced renal function, dose reduction to 250 mg twice daily helps avoid accumulation and toxicity.
The typical course of eight to twelve weeks for acne allows clinicians to assess response while limiting exposure.
If lesions improve markedly after the initial six weeks, consider tapering to a maintenance schedule or switching to a topical agent.
Documenting lesion size and patient‑reported side effects at day 7 and day 14 provides objective data for future treatment decisions.
In cases of impetigo or cellulitis, obtaining a culture before prescribing can confirm susceptibility and prevent unnecessary broad‑spectrum use.
When resistance patterns in the community are high, combining oral tetracycline with benzoyl peroxide can reduce bacterial load and delay resistance.
Patients should be warned about the rare but serious risk of intracranial hypertension, especially women of child‑bearing age, and instructed to seek immediate care for persistent headaches.
For children under eight, avoid tetracycline altogether; the risk of permanent tooth discoloration outweighs any antimicrobial benefit.
Finally, reinforce adherence by setting realistic expectations – improvement is gradual, and stopping the drug early only fuels resistance.
Tristan Francis
October 18, 2025 AT 20:20Tetracycline is cheap and works for many skin bugs. But big pharma hides the resistance data.
Keelan Walker
October 25, 2025 AT 13:16Hey folks 😊, if you’re starting tetracycline make sure you space out calcium intake – two hours is the sweet spot ⏰. Also, a good sunscreen isn’t optional, it’s a must‑have 😎. For acne patients, I usually suggest a follow‑up at six weeks to gauge progress 📈. Remember to drink plenty of water with each dose to avoid esophageal irritation 💧. And if you notice any weird rash, drop the med and call your doctor ASAP 🚑.
Heather Wilkinson
November 1, 2025 AT 05:13Great rundown! 🌟 Just a quick tip: adding a probiotic when you’re on antibiotics can help keep your gut flora balanced 🤗.
Henry Kim
November 7, 2025 AT 22:09I appreciate the thoroughness of this guide. It’s helpful to have clear checkpoints for liver function and renal dosing.
Neha Bharti
November 14, 2025 AT 15:06The balance between efficacy and stewardship is the ethical core of antibiotic use.
Samantha Patrick
November 21, 2025 AT 08:02Yo, dont forget to tell patients that milk can mess up the med absorption – skip dairy for a couple hrs.
Ryan Wilson
November 28, 2025 AT 00:59It’s a shame that some doctors think “cheap” means “cut corners”. Skipping the culture step just to save a few bucks increases resistance, which ends up costing more in the long run. If you’re prescribing tetracycline without confirming susceptibility, you’re basically gambling with patient health. Think before you write that prescription.
EDDY RODRIGUEZ
December 4, 2025 AT 17:55Listen up, team! Tetracycline can be a lifesaver, but only if you respect its limits. Ignoring the sun‑sensitivity warning is like walking into a wildfire without a mask. When you pair it with benzoyl peroxide, you’re not just treating acne – you’re striking back at resistance. So gear up, follow the protocol, and watch those breakouts vanish!
Christopher Pichler
December 11, 2025 AT 10:52Ah yes, the ever‑glamorous world of tetracycline pharmacodynamics – a masterclass in bacteriostatic machinations. In practice, the MIC thresholds often dictate whether you stay in the therapeutic window or veer into sub‑optimal exposure. Of course, real‑world adherence rarely matches the ideal PK/PD models, but that’s just the fun of clinical decision‑making. Bottom line: know your PK, respect the PD, and avoid the dreaded C. difficile nightmare.
VARUN ELATTUVALAPPIL
December 18, 2025 AT 03:48Attention, all healthcare providers, who prescribe tetracycline: please, ensure that you schedule a follow‑up appointment, preferably within seven days, and, critically, review the patient's medication list for potential chelating agents, such as calcium or iron supplements, because, as research shows, these can reduce absorption by up to fifty percent, leading to sub‑therapeutic levels, and, consequently, treatment failure.
April Conley
December 24, 2025 AT 20:45Tetracycline isn’t for pregnant women. Use doxycycline instead.
Sophie Rabey
December 31, 2025 AT 13:41Sure, because who needs a thorough risk assessment when you can just slap on a cheap antibiotic and hope for the best, right? #sarcasm.
Bruce Heintz
January 7, 2026 AT 06:38Thanks for the detailed guide! :) It’ll definitely help me counsel my patients better.
richard king
January 13, 2026 AT 23:34Behold, the double‑edged sword of tetracycline-simultaneously a healer and a harbinger of resistance, a phoenix rising from the ashes of bacterial conquest, yet lurking in the shadows of phototoxic peril. Embrace its power wisely, lest you summon the wrath of unforeseen side effects.