Every year, over 100,000 people in the U.S. die from preventable drug reactions. Many of these deaths happen because someone took a new pill, supplement, or even a common painkiller without knowing it clashed with something they were already taking. It’s not always the doctor’s fault. Often, the patient didn’t know to tell them about the fish oil, the turmeric capsule, or the over-the-counter sleep aid they’ve been using for months. Medication list sharing isn’t just a good idea-it’s a life-saving habit.
What Makes a Medication List Complete?
A simple list of names won’t cut it. A full medication list includes every substance you put into your body, not just prescriptions. That means:- Brand and generic names (e.g., “Lisinopril 10 mg” or “Zestril 10 mg”)
- Dosage and how often you take it (e.g., “once daily,” “every 8 hours”)
- Route (oral, topical, injection, etc.)
- Why you’re taking it (e.g., “for high blood pressure,” “for joint pain”)
- When you started and who prescribed it
- Special instructions (e.g., “take on empty stomach,” “avoid grapefruit,” “take with food”)
And don’t forget the stuff people assume doesn’t matter:
- Over-the-counter meds: Tylenol, ibuprofen, antacids, cold pills
- Vitamins and minerals: Vitamin D, iron, magnesium
- Herbal supplements: St. John’s Wort, garlic pills, ginkgo biloba
- Supplements you got from a friend or bought online
- Allergies and reactions: Not just “penicillin allergy,” but “hives, swelling, trouble breathing”
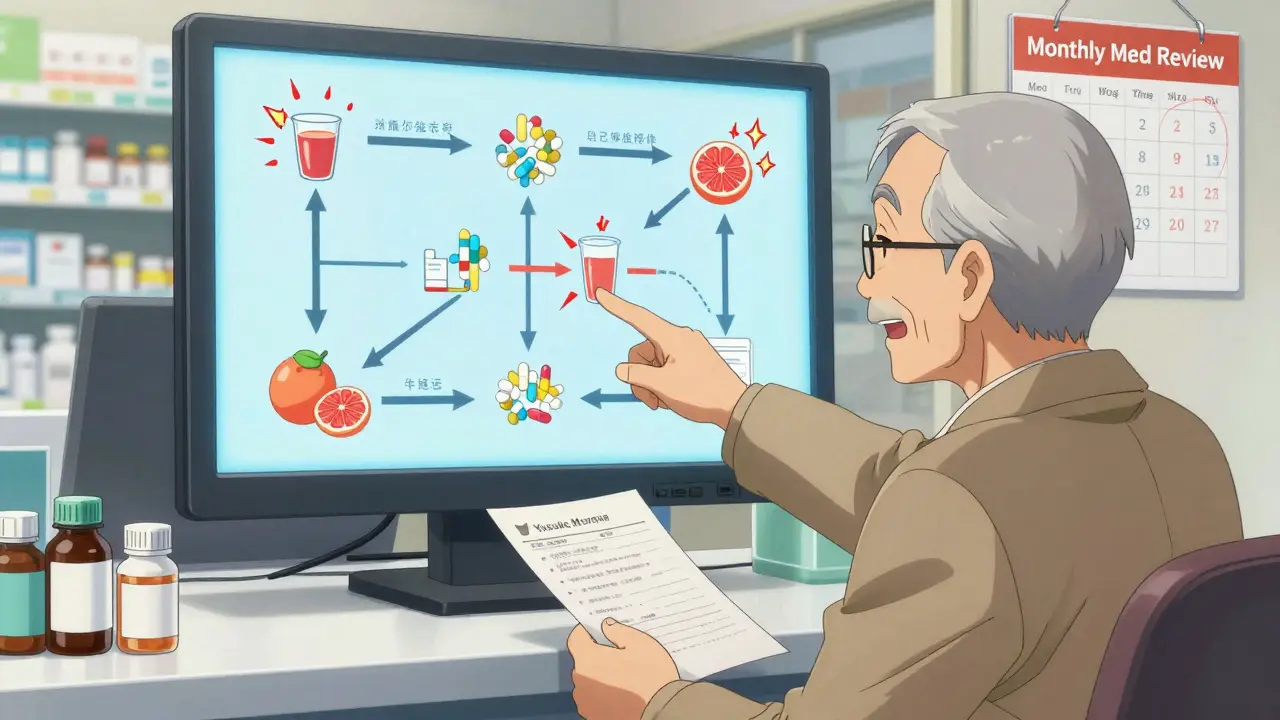
Why? Because St. John’s Wort can make your blood thinner useless. Calcium supplements can block your thyroid medicine. Even something as simple as grapefruit juice can turn a common statin into a dangerous toxin. The FDA found that 30% of serious drug interactions involve these “harmless” items.
Why Paper Lists Fail-and Digital Ones Can Too
You’ve probably seen someone pull out a folded piece of paper from their wallet with a messy list written in pen. It’s better than nothing, but it’s outdated. A 2022 study found paper lists are only 62% accurate in emergencies. Why? Because people forget to update them. They add a new pill, forget to cross out the one they stopped, and the list becomes a liability.Digital lists on apps like Medisafe or MyMeds are more accurate-78% in one study-but they only work if you have a smartphone and remember to update them. And here’s the catch: even the best app won’t help if your doctor’s system doesn’t see it. Most electronic health records (EHRs) capture only 52% of over-the-counter meds and 38% of supplements. That’s not a system failure-it’s a communication gap.
The most effective method? A combo approach:
- Keep a digital list on your phone (updated within 24 hours of any change)
- Take a photo of every pill bottle in your medicine cabinet
- Print a clean, one-page summary to carry with you
When you walk into a clinic, hand them the printed list before they even ask. Don’t wait. Only 37% of providers routinely request a full list, according to MedlinePlus.
Who Needs This Most-and Why
If you’re over 65, you’re not alone. About 40% of older adults take five or more medications. The average is 4.8 prescriptions per person, up from 3.1 in 2010. With more meds comes more risk. People taking five or more drugs have 87% higher chances of a dangerous interaction.But it’s not just seniors. Anyone seeing multiple specialists-cardiologist, endocrinologist, neurologist-is at risk. Each doctor sees their piece of your health, not the whole picture. One doctor prescribes a new antidepressant. Another adds a painkiller. Neither knows the third prescribed a blood pressure med that reacts badly with both. That’s how you end up in the ER.
Experts like Dr. Robert W. Hardy at Harvard say: “Failure to share a complete medication list is the single most preventable cause of adverse drug events.” That’s not a guess. That’s based on data from thousands of cases.
How to Keep Your List Updated
A list that’s six months old is useless. Here’s how to keep it alive:- Update within 24 hours of any change-new prescription, stopped pill, added supplement
- Review every month: Check expiration dates, unused bottles, and whether you still need each item
- Use your pharmacy: If you fill all your prescriptions at one pharmacy, they can flag interactions automatically. Their systems catch 92% of major drug clashes
- Ask your pharmacist: They’re trained to spot these issues. A 2023 study showed pharmacist-led reviews reduced bad prescribing by 32% in older adults
Pro tip: Set a monthly calendar reminder. When it goes off, take out your phone, open your medication app, and go through each bottle. Take a photo of any new one. Cross out anything you stopped. Update the reason if it changed.
What to Say to Your Doctor
Don’t just hand over the list and hope they read it. Say this:- “Could any of these medications interact with each other?”
- “Are there any foods, drinks, or supplements I should avoid?”
- “Is there anything here I don’t need anymore?”
- “Can we go over the timing? I’m not sure if I’m taking them right.”
Some meds need precise timing. Levothyroxine? Take it 30-60 minutes before breakfast, on an empty stomach. Metformin? Take it with meals to avoid stomach upset. Statins? Often best at night. Get it wrong, and the drug won’t work-or worse, it’ll hurt you.
Real Stories, Real Consequences
On Reddit, a woman named “MedSafetyMom” shared how she saved her husband’s life. He was on warfarin for a blood clot. His naturopath recommended St. John’s Wort for “mood support.” The doctor didn’t ask about supplements. The pharmacist didn’t know. She found out because she kept a full list. When she showed it to her cardiologist, he immediately stopped the supplement. The interaction could have caused a deadly clot.On the flip side, 68% of patients on PatientsLikeMe said their providers rarely asked for their full list. Over half said they forgot to mention their vitamins or OTC meds. That’s not negligence-it’s a system failure. And it’s fixable.
What’s Changing in 2026
The government is pushing for change. The 21st Century Cures Act now requires health records to include patient-reported medication data. New tools like IBM Watson’s AI checker can detect 94% of dangerous interactions. By 2026, most digital health systems will automatically pull in your supplement list if you enter it.But until then, the power is in your hands. You are the only person who knows every pill, every drop, every capsule you’ve taken in the last six months. No app, no doctor, no pharmacy can know that unless you tell them.
Start Today: Your 5-Minute Action Plan
You don’t need a fancy app. Just do this now:- Open your medicine cabinet. Take a photo of every bottle-prescription, OTC, vitamin, supplement.
- Write down: name, dose, frequency, reason, start date, prescriber.
- Include everything-even the aspirin you take once a week.
- Print one copy. Put it in your wallet. Save a digital copy on your phone.
- Next time you see a doctor, hand it to them before they sit down.
It’s not complicated. It’s not expensive. It’s not optional. If you take more than one thing, you need this list. It’s your shield against something that could kill you.
What if I forget to update my medication list?
Set a monthly phone reminder. Every first of the month, spend five minutes checking your bottles and updating your list. If you’re on a new med, update it within 24 hours. Waiting longer makes your list unreliable. Outdated lists are one of the top causes of dangerous interactions-52% of errors come from not updating.
Do I really need to include vitamins and supplements?
Yes. Supplements aren’t harmless. St. John’s Wort can make birth control, antidepressants, and blood thinners fail. Garlic pills can thin your blood too much when combined with warfarin. Even high-dose Vitamin E can interfere with chemotherapy. The FDA says 30% of serious interactions involve these items. If you’re taking it, it belongs on the list.
Can my pharmacist help me with my medication list?
Absolutely. Pharmacists are trained to spot interactions you and your doctor might miss. If you fill all your prescriptions at one pharmacy, they’ll automatically screen for clashes. Many offer free medication reviews-ask for one. A 2023 study showed pharmacist-led reviews cut bad prescribing by 32% in older adults. They’ve seen it all.
What if my doctor doesn’t look at my list?
Hand it to them before they sit down. Say, “I’ve updated my list and wanted to make sure we’re not missing anything.” Most providers won’t ask, but they’ll look if you hand it to them upfront. If they ignore it, ask directly: “Could any of these interact?” If they still don’t engage, consider finding a provider who takes safety seriously.
Is there a free template I can use?
Yes. The FDA offers a free “My Medicine Record” form online. The American Academy of Family Physicians also has a printable template. Use either. Or just use a plain piece of paper. The format doesn’t matter-completeness does. Just make sure it includes all meds, doses, reasons, and allergies.
What to Do Next
If you take more than one medication, stop reading and do this now: open your medicine cabinet. Take a photo of every bottle. Write down what’s in them. Print one copy. Put it in your wallet. Save one on your phone. Next time you see a doctor, hand it to them before they say “How are you?”This isn’t about being organized. It’s about staying alive. You don’t need to be an expert. You just need to be the one who speaks up.

Jake Moore
January 19, 2026 AT 02:35Just did this right now - took pics of every bottle in my cabinet, wrote down names, doses, and why I’m taking them. Even included the gummy vitamins I thought were ‘harmless.’ Printed it, saved it on my phone, and put a copy in my wallet. Feels weirdly empowering, like I just armed myself against a silent killer.
Thanks for the nudge. I’m telling my cardiologist next Tuesday - before he even sits down.
Praseetha Pn
January 19, 2026 AT 06:01LOL you think this is about meds? Nah. Big Pharma doesn’t want you to know that 90% of these ‘interactions’ are made up so they can sell you *new* drugs to fix the side effects of the *old* drugs they sold you. They profit from chaos. St. John’s Wort? They call it ‘dangerous’ because it’s cheap and you can buy it at Walmart. Meanwhile, their $800-a-pill ‘innovative’ antidepressant? Totally safe. Right.
And don’t get me started on how your ‘pharmacist’ is just a corporate drone trained to shut you up with ‘follow your script.’ They don’t care if you live or die - only if you refill.
Nishant Sonuley
January 20, 2026 AT 01:16Look, I get it - lists are good. But let’s be real: if your doctor’s EHR can’t even pull in your OTC meds, what’s the point of you doing all this work? It’s like polishing a shoe while the car’s on fire.
Still, I do it. Not because I trust the system - I don’t - but because I’m tired of being treated like a puzzle piece that doesn’t fit. I keep a digital list, a printed one, and a photo of every bottle. And when my endo says ‘We’ll monitor your levels,’ I say ‘Great. Here’s the list. Also, I stopped the magnesium last month - crossed it out.’
It’s exhausting, but someone’s gotta be the adult in the room. And it ain’t gonna be the 12-minute appointment.
Emma #########
January 20, 2026 AT 14:24This hit me hard. My mom almost went into renal failure last year because she was taking ibuprofen daily for her knees and didn’t tell her nephrologist. She thought it was ‘just painkillers.’
I cried reading this. I’m going to help her update her list this weekend. No more assumptions. No more ‘it’s not a big deal.’
Thank you for saying this so clearly.
Andrew Short
January 21, 2026 AT 21:01People like you are why medicine is broken. You think writing down ‘vitamin D’ is going to save someone? Wake up. The real problem is that doctors are overworked, underpaid, and drowning in paperwork. You’re not saving lives - you’re just adding to the administrative hell.
And don’t get me started on ‘pharmacists’ - they’re just glorified cashiers with a pharmacy degree. They don’t know anything about your liver enzymes or your genetic metabolism.
Stop pretending this is a fix. It’s a Band-Aid on a hemorrhage.
Robert Cassidy
January 22, 2026 AT 12:14Let’s be honest - this isn’t about safety. It’s about control. Who gets to decide what you put in your body? The FDA? The AMA? The guy who owns the pharmacy chain?
You think your ‘med list’ makes you free? Nah. It makes you a compliant sheep, handing over your autonomy to a system that’s designed to keep you dependent.
I stopped taking all meds 3 years ago. I eat turmeric, drink lemon water, and sleep on the floor. I’m healthier than 90% of you with your ‘lists’ and your ‘apps.’
Wake up. The real poison is the belief that you need permission to be well.
Andrew Qu
January 23, 2026 AT 07:14Just want to say - this is one of the most practical, life-saving pieces of advice I’ve seen in a long time.
I’ve been a nurse for 18 years. I’ve seen too many ER visits because someone didn’t mention their fish oil or their herbal tea. One guy took melatonin with his blood thinner - ended up in ICU.
Don’t overcomplicate it. Take a photo. Write it down. Hand it over. It takes 5 minutes. That’s less time than you spend scrolling Instagram.
You’re not being ‘annoying’ - you’re being smart. And if your doctor rolls their eyes? Find a new one. Your life isn’t a suggestion.
Jodi Harding
January 25, 2026 AT 03:50My grandma died from a drug interaction. She took St. John’s Wort with her blood pressure med. No one asked. No one knew.
I don’t post much. But this? I’m sharing it with everyone I know.
Do the list. Now.
Zoe Brooks
January 27, 2026 AT 02:32Just updated my list! 🙌
Added the CBD oil I’ve been taking for anxiety (didn’t think it counted lol), crossed out the expired melatonin, and took pics of my 7 pill bottles. Saved it in my Notes app and printed one.
Feels like I just did my first real act of self-care. Who knew being organized could feel this good?
Also - I told my doctor ‘I’ve got a list’ before he even opened his mouth. He looked surprised. Then he smiled. 😊
Kristin Dailey
January 28, 2026 AT 11:58USA: 100k deaths a year from meds. India? 10x that and no one cares. Your system is broken. Fix your own house before lecturing the world.
Selina Warren
January 28, 2026 AT 21:43Let me tell you - this isn’t just about pills. It’s about power. Who gets to decide what’s ‘medicine’ and what’s ‘supplement’? The FDA? Big Pharma? The same people who told us smoking was safe?
My uncle took 12 meds. He didn’t know half of them were for things he didn’t even have. His doctor was just trying to ‘manage’ him - not heal him.
So I made him a list. He stopped 6 meds. He’s sleeping better. His blood pressure dropped. He’s 78 and walking without a cane.
It’s not magic. It’s just asking the right questions.
You’re not a patient. You’re a person. Act like it.
Robert Davis
January 29, 2026 AT 06:22Yeah, I’ve got the list. I’ve got the app. I’ve got the printed copy. I’ve got the photos.
But here’s the thing - my doctor’s EHR still doesn’t recognize half the supplements. So I just… stop talking. I hand it over. I wait. I watch. I see if they even glance at it.
Most don’t.
So I’ve stopped trusting the system. I’ve started trusting myself. And I’ve started seeing a functional medicine doc who actually asks about my turmeric.
It’s not about being ‘difficult.’ It’s about surviving a system that doesn’t care if you live.
Eric Gebeke
January 30, 2026 AT 01:10People like you are the reason I hate modern medicine.
You treat your body like a spreadsheet. ‘List your meds.’ ‘Update your app.’ ‘Print your sheet.’
What happened to listening to your body? To intuition? To natural healing?
You’ve outsourced your health to algorithms and corporate pharmacies.
And now you’re proud of it?
Pathetic.