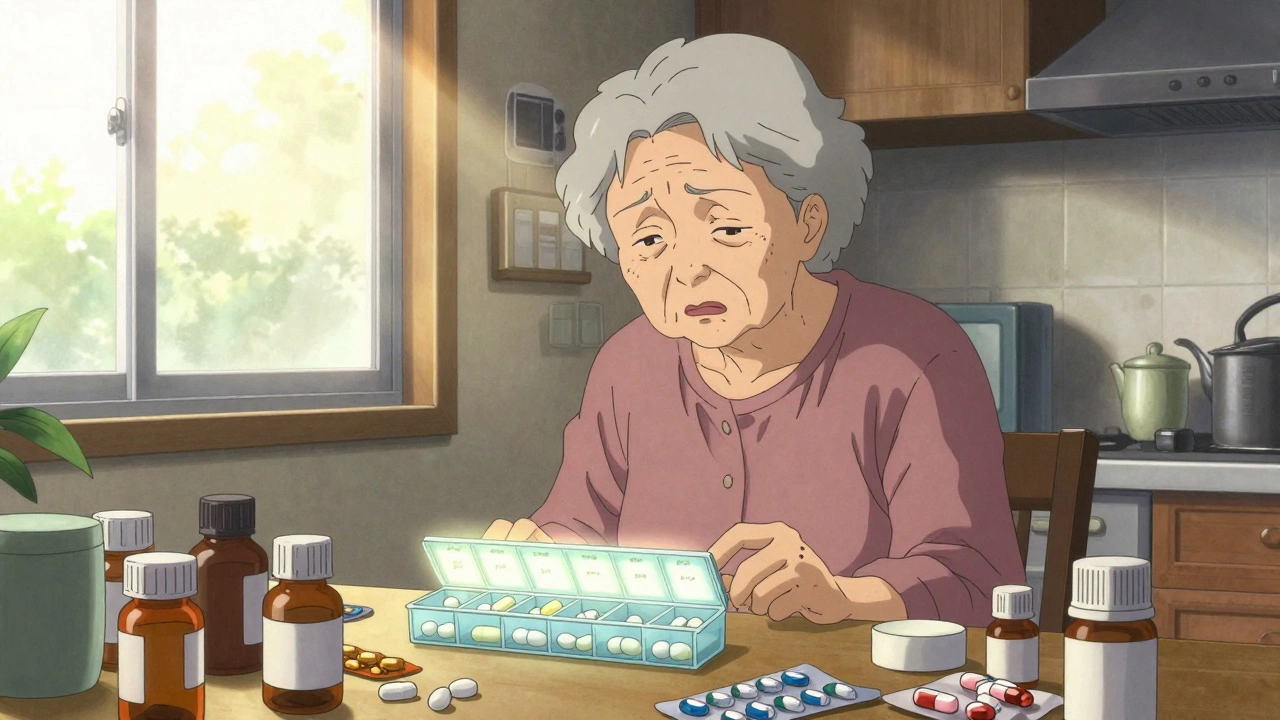
Imagine waking up every morning to a kitchen counter covered in pill bottles-some for blood pressure, others for cholesterol, diabetes, arthritis, and more. By noon, you’ve swallowed 8 pills. By bedtime, it’s 12. And you’re not even sure if you took the right one at the right time. This isn’t rare. For older adults taking five or more medications, this daily ritual is normal. But it’s also dangerous. The more pills you have to manage, the more likely you are to miss a dose, take the wrong one, or stop altogether. The good news? You don’t need to keep doing it this way. Simplifying your medication schedule with fewer daily doses isn’t just convenient-it’s backed by science, and it works.
Why Fewer Doses Mean Better Adherence
It’s not about laziness. It’s about human biology. Our brains aren’t wired to remember 12 different times a day to take pills. Studies show that when people take medications four or more times daily, adherence drops below 50%. But when dosing is reduced to once or twice a day, adherence jumps to 75% or higher. That’s not a small difference-it’s the difference between controlling your blood pressure and ending up in the hospital.
The key insight? Medication adherence isn’t about willpower. It’s about design. If your schedule is too complicated, your brain will drop the ball-even if you care deeply about staying healthy. That’s why simplifying your regimen isn’t just a suggestion. It’s a medical strategy.
How to Cut Down Your Daily Doses
There are four proven ways to reduce the number of times you take pills each day. None require you to stop taking your medications. They just make the process smarter.
- Fixed-dose combinations (FDCs): This is when two or more drugs are combined into one pill. For example, instead of taking a blood pressure pill and a cholesterol pill separately, you might get a single pill that contains both. About one-third of all successful simplifications use this method. It’s especially common in HIV and heart disease treatment, where combining drugs has been shown to boost adherence by up to 25%.
- Once-daily dosing: Some medications come in extended-release forms that last 24 hours. If you’re taking a drug three times a day, ask your doctor if a once-daily version exists. This works well for blood pressure, depression, and diabetes meds. But not all drugs can be converted-some need to be taken multiple times to stay effective. Your pharmacist can check if yours can be switched.
- Medication synchronization: This means getting all your prescriptions filled on the same day each month. Instead of visiting the pharmacy every few weeks for different meds, you get everything at once. This cuts down on missed doses caused by running out of one pill while waiting for another. Patients using this method reduce pharmacy visits by 60% and cut gaps in treatment by nearly half.
- Multi-dose compliance packaging: Think of it like a weekly pill organizer with compartments for morning, noon, evening, and bedtime. Pharmacists fill these with your exact doses for the whole week. Studies show this improves adherence by 22% compared to loose bottles. For seniors with memory issues, it’s a game-changer.
The Universal Medication Schedule recommends organizing all meds into just four daily time slots: morning, noon, evening, and bedtime. Right now, nearly 30% of patients take meds seven or more times a day. Shifting to four slots cuts confusion and errors by 35%.
What Works-and What Doesn’t
Not every medication can be simplified. Some drugs need to be taken at specific times because of how they work in your body. For example, insulin or certain antibiotics must be timed precisely. But for many chronic conditions-like high blood pressure, cholesterol, diabetes, and arthritis-there’s room to consolidate.
Fixed-dose combinations are powerful, but only if the doses match up. You can’t combine two drugs if one needs to be taken at 50 mg and the other at 100 mg, and no combo exists at that ratio. Once-daily versions are great, but insurance often denies them because they’re more expensive. About 45% of patients on Medicare Advantage face coverage denials for these preferred formulations.
Multi-dose packaging works wonders for elderly patients, but it costs 15-20% more than regular bottles. If you’re on a tight budget, ask your pharmacist if your state offers free or low-cost compliance packaging programs. Many do.
And here’s the catch: simplification doesn’t always mean better health outcomes. One study found that even though HIV patients took their meds more consistently after switching to once-daily regimens, their viral load didn’t improve further. That’s because they were already doing okay. The real win? Fewer missed doses, less stress, and more freedom.

How to Start the Process
You don’t need to figure this out alone. Here’s a step-by-step plan you can take to your doctor or pharmacist:
- Make a complete list of every medication you take, including over-the-counter pills, vitamins, and supplements. Write down the dose and how often you take it.
- Bring it to your appointment. Ask: “Can any of these be combined or switched to once-daily versions?” Don’t be shy. This is a standard part of care for older adults.
- Ask about synchronization. Can all my refills be due on the same day each month? Many pharmacies offer this for free.
- Request a pill organizer. If you’re taking five or more meds, ask if your pharmacy offers pre-filled compliance packaging. Some even deliver them to your door.
- Review with a pharmacist. Pharmacists are medication experts. Schedule a Medication Therapy Management (MTM) session-it’s covered by Medicare and many private plans.
The whole process takes less than an hour. But the payoff lasts for months-or years.
Common Barriers and How to Overcome Them
Even when simplification makes sense, obstacles get in the way.
- Insurance won’t cover the new pill: If your doctor recommends a fixed-dose combo but your plan denies it, ask for a prior authorization. If that fails, ask for a therapeutic substitution-sometimes a different brand with the same effect is covered.
- You’re afraid of mixing pills: Many patients worry that combining meds could cause dangerous interactions. But pharmacists check for this before any change. If you’re unsure, ask: “Is this safe to take together?”
- Your doctor doesn’t bring it up: Most primary care doctors are busy. Don’t wait for them to suggest it. Bring it up yourself. Say: “I’m struggling to keep up with my pills. Can we make this simpler?”
- Family members don’t help: If you live with someone, show them your pill organizer. Ask them to check in once a week. A simple reminder can prevent a missed dose.
One caregiver on AgingCare.com said: “My mom went from 12 bottles to one organizer. She stopped asking what day it was. She stopped forgetting her meds. It felt like she got her memory back.”

What’s Changing in 2025
The field is evolving fast. In 2022, the FDA approved 12 new fixed-dose combination drugs-25% more than in 2020. More are coming. Smart pill dispensers that send alerts to your phone or caregiver are now being tested in Medicare Advantage plans. AI tools can now scan your entire medication list and suggest possible simplifications in seconds.
Medicare now covers annual medication reviews as part of the Annual Wellness Visit. That means your doctor is supposed to ask you about your pill routine every year. If they don’t, remind them. You have the right to ask.
Still, the biggest barrier isn’t technology-it’s awareness. Only 35% of primary care practices regularly use simplification tools. Hospitals do it more often, especially when patients are discharged. But at home? You have to push for it.
Real Results, Real People
A 72-year-old man with hypertension, diabetes, and high cholesterol was taking 11 pills a day. After switching to two fixed-dose combinations and using a weekly organizer, he dropped to four pills total-two in the morning, two at night. His adherence went from 58% to 92%. He started walking again. He stopped going to the ER.
A woman in her 60s with depression and arthritis was taking seven meds at five different times. She started missing doses because she couldn’t keep track. After switching to once-daily versions and using synchronized refills, she went from missing 3-4 doses a week to none. “I finally feel like I’m in control,” she said.
These aren’t rare cases. They’re the rule when simplification is done right.
Next Steps: What to Do Today
You don’t need to wait for your next appointment. Here’s what you can do right now:
- Write down every medication you take, including doses and times.
- Call your pharmacy and ask: “Do you offer medication synchronization or pre-filled pill organizers?”
- Look up your medications online. Search “[Drug Name] once daily version.” See if alternatives exist.
- Print this list and bring it to your next doctor visit. Say: “I want to simplify my regimen. Can we make this easier?”
Simplifying your medication schedule isn’t about cutting corners. It’s about working smarter. Fewer pills. Fewer mistakes. More peace of mind. And better health-not because you’re trying harder, but because your system finally works for you.

Ella van Rij
December 2, 2025 AT 00:43Oh wow, finally someone wrote a 2000-word essay on not forgetting your pills. I was starting to think the only solution was to glue them to my forehead. 🙃
Rebecca M.
December 3, 2025 AT 07:05My grandma took 14 pills a day and still remembered which was which. She didn’t need a fancy organizer-she had willpower. People these days act like taking a pill is rocket science. It’s just swallowing a tiny rock. Why are we treating seniors like toddlers now?
Alicia Marks
December 4, 2025 AT 00:00You got this. One step at a time. Even just writing down your meds is a huge win. You’re already ahead of 90% of people who just guess what’s in that bottle. 💪
Paul Keller
December 5, 2025 AT 03:01While the article presents a compelling case for medication simplification, it is important to acknowledge the systemic underpinnings of pharmaceutical complexity. The fragmentation of care, lack of interprofessional coordination, and profit-driven formulary decisions by insurance entities are the true root causes of polypharmacy burdens. The proposed solutions-while pragmatically useful-are symptomatic palliatives. True reform requires pharmacoeconomic restructuring, not merely behavioral adaptation. That said, the four strategies enumerated are clinically sound and represent the best available tools within a broken system.
Roger Leiton
December 7, 2025 AT 01:01This is so helpful!! 🙌 I just got my mom’s meds synced last month and she’s been so much calmer. She even started painting again-something she hadn’t done in years. The pill organizer? Total game changer. Also, I had no idea Medicare covers MTM sessions. Going to call my pharmacist tomorrow. Thanks for this!! 🌟
Laura Baur
December 8, 2025 AT 11:12Let us not be fooled by the seductive simplicity of this narrative. The notion that adherence can be ‘engineered’ through packaging or combination pills is a neoliberal fantasy that absolves individuals of responsibility while obscuring the deeper moral failure of a healthcare system that normalizes pharmaceutical overprescription. Why are we medicating every discomfort? Why are we outsourcing cognitive function to pill organizers? The real crisis isn’t the number of pills-it’s the surrender of autonomy to a pharmacological regime disguised as care. You are not a machine to be optimized. You are a human being who deserves to understand why you take what you take-not just when.
Jack Dao
December 9, 2025 AT 23:20Wow. Another one of those ‘just ask your doctor’ articles. As if doctors have time to sit through your 27-medication spreadsheet. And don’t get me started on ‘synchronized refills’-try getting that in rural Iowa. This reads like a pharmaceutical marketing pamphlet disguised as public health advice. Also, who wrote this? Someone who’s never had to wrestle with a pharmacy phone tree? 😒
dave nevogt
December 11, 2025 AT 11:36I’ve watched my father navigate this for years. He never complained, but I saw the exhaustion-the way he’d stare at the pillbox for minutes, unsure if he’d already taken the blue one. It wasn’t forgetfulness. It was grief. Grief for the life he used to have, before the pills became his schedule, his identity, his burden. The tools mentioned here-FDCs, organizers, sync-aren’t just practical. They’re acts of dignity. They give back a sliver of control. And sometimes, that’s all you need to breathe again.