JAK inhibitors are changing how we treat autoimmune diseases like rheumatoid arthritis, psoriasis, and alopecia areata. These pills don’t just ease symptoms-they stop the immune system from attacking the body at its core. But they’re not harmless. For every patient who sees their skin clear or joints stop aching, another faces shingles, high cholesterol, or worse. The key isn’t just taking the pill-it’s knowing who should take it, who shouldn’t, and how to watch for trouble before it’s too late.
How JAK Inhibitors Actually Work
Unlike biologic drugs that target single proteins like TNF or IL-17, JAK inhibitors go deeper. They block enzymes inside immune cells called Janus kinases-JAK1, JAK2, JAK3, and TYK2. These enzymes act like switches that turn on inflammation when cytokines signal danger. When a JAK inhibitor binds to one of these switches, it stops the signal from reaching the nucleus. No signal means no inflammatory genes get turned on. That’s why one pill can calm down multiple conditions at once: rheumatoid arthritis, eczema, and even hair loss from alopecia areata.
Some JAK inhibitors are picky. Upadacitinib targets JAK1 more than JAK2, which helps reduce side effects. Abrocitinib is even more selective, with an IC50 of just 0.029 μM for JAK1. Others, like baricitinib, hit JAK1 and JAK2 harder, which can mean stronger results but also more risks. Then there’s ritlecitinib, which binds permanently to JAK3 like a lock and key-it doesn’t just block, it disables. This precision matters because JAK2 controls red blood cell production, and JAK3 is key for T-cell function. Mess with the wrong one, and you get anemia or a weakened immune system.
Why Patients Love Them
Patients don’t need shots. No more freezing needles before bedtime. No more clinic visits just to get an infusion. A simple daily pill fits into life. In a survey of over 1,200 people with autoimmune conditions, 92% preferred JAK inhibitors over injections. Speed matters too. While TNF blockers take 8 to 12 weeks to show results, many patients report feeling better in 2 to 4 weeks. One user on HealthUnlocked said baricitinib dropped their swollen joints from 18 to 2 in just six weeks. Another said abrocitinib cleared their eczema in 10 days.
That speed and convenience explain why JAK inhibitors now make up about 25% of the rheumatoid arthritis treatment market. In the U.S., 32% of rheumatologists prescribe them as first-line after methotrexate fails. That’s up from just 8% five years ago. The global market hit $12.3 billion in 2023 and is expected to grow over 8% yearly through 2030.
The Hidden Risks
But here’s what no one tells you at first: these pills come with a black box warning-the strongest the FDA can give. In January 2022, the agency updated labels to highlight four major dangers: serious infections, cancer, heart attacks, and blood clots. The ORAL Surveillance study followed over 4,000 rheumatoid arthritis patients for years. Those on tofacitinib had a 31% higher risk of major heart events and a 49% higher risk of cancer compared to those on TNF inhibitors. That’s not a small number. It’s enough to make doctors pause before prescribing.
One of the most common side effects isn’t cancer or heart trouble-it’s shingles. About 23% of patients on JAK inhibitors get herpes zoster reactivation. That’s nearly eight times higher than with biologics. Many now take daily antivirals like valacyclovir as prevention. Another frequent issue? Cholesterol. Nearly half of users see their LDL jump by 20 to 30 mg/dL. One Reddit user reported his went from 110 to 138 in three months. That’s enough to push someone into high-risk territory for heart disease.
Who Shouldn’t Take Them
Not everyone is a candidate. The European League Against Rheumatism (EULAR) and American College of Rheumatology (ACR) guidelines are clear: avoid JAK inhibitors in patients over 65 with heart disease, smokers, those with a history of cancer, or anyone with low lymphocyte counts. If your LDL is above 190 mg/dL, you need a statin before starting. If your hemoglobin drops below 8 g/dL, you stop. If your liver enzymes spike past three times normal, you’re off the drug.
Patients with untreated tuberculosis are also at high risk. That’s why every person starting a JAK inhibitor must get a TB skin test or blood test first. Even then, some cases reactivate. The European Medicines Agency recommends getting the shingles vaccine at least four weeks before starting-but only 68% of clinics in Europe do this consistently. Too many patients are rushed into treatment because their symptoms are bad, and the urgency overrides caution.
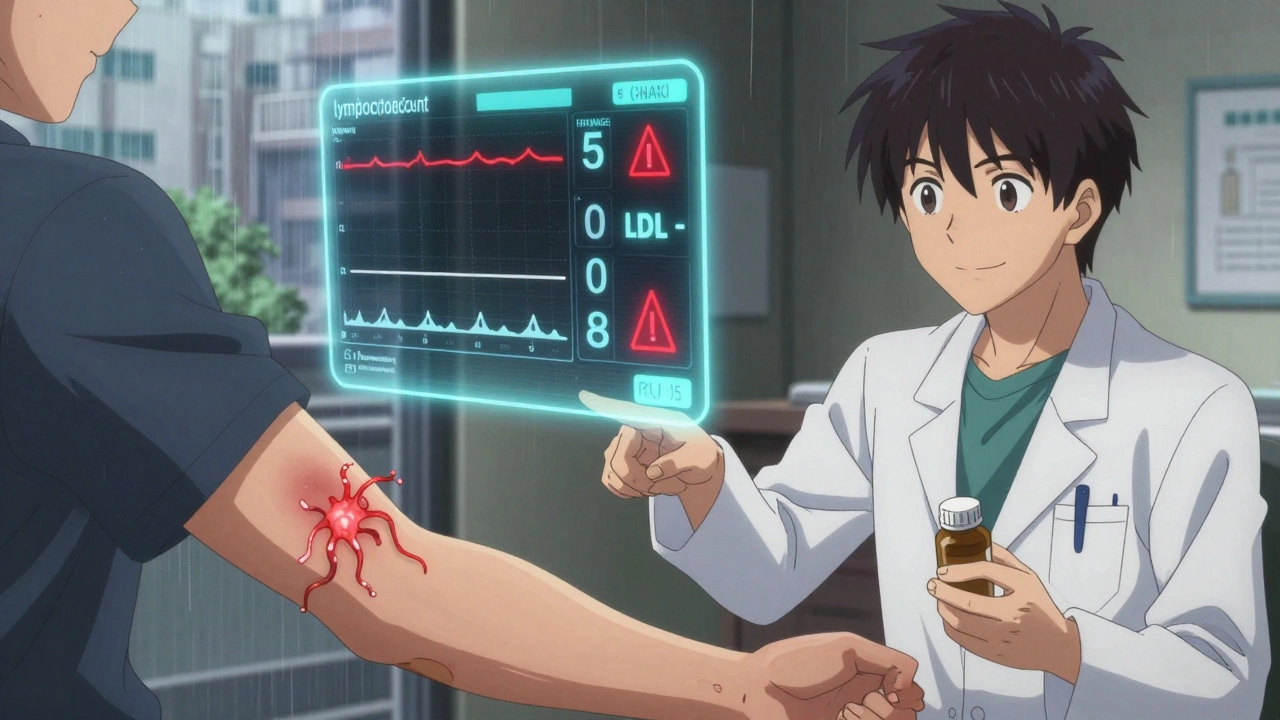
What to Monitor and When
Monitoring isn’t optional. It’s part of the treatment. The ACR 2023 guidelines say you need baseline blood work before the first pill: CBC, liver enzymes, lipid panel, and TB screen. Then, every three months for the first year. After that, every six months. But many patients stop coming in after six months. That’s when problems sneak in.
Here’s what to check each visit:
- Absolute lymphocyte count: if it falls below 500 cells/μL, stop the drug
- Hemoglobin: if it drops below 8 g/dL, investigate anemia
- ALT/AST: if over 3x upper limit, pause and retest
- LDL cholesterol: if above 190 mg/dL, start a statin
- Herpes zoster symptoms: red, painful rash? Treat immediately
Doctors report a 3- to 6-month learning curve to manage these numbers well. Some start patients on low-dose statins upfront. Others prescribe antivirals prophylactically. The goal isn’t to scare people off-it’s to keep them safe while they benefit.
New Drugs on the Horizon
The next wave of JAK inhibitors is trying to fix the safety problems. Deuruxolitinib, approved in June 2024 for alopecia areata, requires strict monitoring and enrollment in a REMS program. Brepocitinib, a TYK2 inhibitor, is in phase 3 trials and expected to finish in mid-2025. TYK2 is more selective-it blocks fewer pathways, meaning fewer side effects. Early data shows it works for psoriasis and lupus without the same cholesterol or infection spikes.
Another promising candidate is a JAK3-specific inhibitor that binds irreversibly to the enzyme. This could mean lower doses and less impact on other JAKs. If it works, it might finally deliver the power of JAK inhibition without the risks.
The Bottom Line
JAK inhibitors are powerful. They’ve given people back their skin, their hair, their ability to walk without pain. But they’re not magic. They’re tools-and tools can cut both ways. The best outcomes come from careful selection, strict monitoring, and honest conversations about risk. If you’re considering one, ask your doctor: “Am I a good candidate? What will we check, and how often?” Don’t let convenience override caution. The pill might change your life-but only if you manage it right.
Are JAK inhibitors better than biologics?
It depends. JAK inhibitors work faster and are easier to take because they’re pills, not injections. For patients who hate needles or need quick relief, they’re often better. But biologics have a longer safety track record. If you have heart disease, are over 65, or have had cancer, biologics are usually safer. JAK inhibitors are best for younger, healthier patients without major risk factors.
Can I drink alcohol while taking a JAK inhibitor?
Moderate alcohol is usually okay, but heavy drinking increases liver damage risk. Since JAK inhibitors can raise liver enzymes, combining them with alcohol makes it harder to tell if a spike is from the drug or the booze. Most doctors recommend limiting alcohol to one drink per day or less. If your liver numbers are already high, skip it entirely.
Do JAK inhibitors cause weight gain?
Not directly. But some patients gain weight because their inflammation drops and appetite improves. Others feel better and become more active, which helps them lose weight. Weight changes are individual. The bigger concern is cholesterol, not weight. Monitor lipid levels closely, not the scale.
What happens if I stop taking a JAK inhibitor?
Symptoms often return within weeks. Unlike some biologics, JAK inhibitors don’t reset the immune system-they just suppress it. Stopping suddenly can cause a flare-up. Never quit without talking to your doctor. If you need to stop due to side effects, your doctor may switch you to another drug or taper slowly to avoid rebound inflammation.
Are JAK inhibitors used for conditions other than arthritis?
Yes. They’re FDA-approved for psoriasis, atopic dermatitis, alopecia areata, and ulcerative colitis. Many doctors use them off-label for vitiligo, hidradenitis suppurativa, and even some forms of lupus. A 2023 survey found 43% of dermatologists use them for vitiligo, and 18% for hidradenitis. Research is ongoing for other autoimmune conditions.


Chris Park
December 5, 2025 AT 13:57Let me guess-the FDA’s black box warning is just corporate theater. They’ve been suppressing natural cures for decades while pushing pharmaceuticals that make people dependent. JAK inhibitors? More like JAK-TRAP. You think they care about your joints? They care about your monthly co-pay. The real danger isn’t the drug-it’s the system that profits from your chronic illness. And don’t even get me started on the ‘monitoring’-it’s just a way to keep you coming back for more blood draws and $200 copays.
Inna Borovik
December 7, 2025 AT 09:31Actually, the data from ORAL Surveillance is statistically significant and clinically actionable. The 31% increase in cardiovascular events isn’t noise-it’s a signal. What’s concerning is how many clinicians still treat this like a ‘convenience drug’ instead of a high-risk intervention. The lipid spikes alone should trigger mandatory statin co-prescribing. And yet, we’re seeing patients on JAK inhibitors with LDLs over 200 and zero follow-up. That’s not patient care-that’s negligence dressed up as innovation.
Jackie Petersen
December 7, 2025 AT 15:19Oh please. You people act like this is the first time Big Pharma ever sold poison with a smile. Remember Vioxx? Thalidomide? Opioids? This is just the same script with new labels. They’ll market these pills as ‘miracle cures’ until someone dies, then quietly bury the data and move on to the next ‘breakthrough.’ Meanwhile, your grandma’s turmeric tea and acupuncture are still out there working quietly-no FDA warning needed.
Annie Gardiner
December 8, 2025 AT 18:12I get why people are excited-finally, a pill that works fast, no needles, no clinic trips. But… it’s like falling in love with someone who’s beautiful but secretly dangerous. You ignore the red flags because the highs are so good. I started one for my eczema. My skin cleared in two weeks. Then my cholesterol went nuts. I felt guilty taking it. Like I was betraying my body for a quick fix. I’m off it now. Not because I’m scared-because I realized I didn’t want to live in a body that needed a chemical leash to be whole.
Myles White
December 10, 2025 AT 11:43There’s a lot of nuance here that’s being lost in the fear-mongering. JAK inhibitors aren’t inherently bad-they’re powerful tools that require precision, not panic. The key is risk stratification: younger patients with no cardiovascular history, normal lipids, and no cancer risk? They’re ideal candidates. Older patients with comorbidities? Stick with biologics. The real issue isn’t the drug-it’s the lack of standardized monitoring protocols across practices. I’ve seen patients get baseline labs and then vanish for a year. That’s not the drug’s fault-it’s the system’s failure. We need mandatory EHR alerts for lipid and lymphocyte trends, automated reminders for TB retesting, and integration with pharmacy data to flag concurrent antivirals. This isn’t rocket science-it’s basic clinical workflow optimization.
Saketh Sai Rachapudi
December 11, 2025 AT 22:55USA thinks it owns medicine now? JAK inhibitors? I saw this in India 10 years ago-pharma companies push these pills to rich people while poor get nothing. You think this is science? No. This is capitalism with a stethoscope. We have Ayurveda that heals without killing cholesterol. You Americans are so addicted to pills you forget your body can heal itself. And now you want to export this poison to the world? Shame.
joanne humphreys
December 13, 2025 AT 04:43I’ve been on baricitinib for 14 months. My RA went from debilitating to barely noticeable. I still get my labs every 3 months-CBC, lipids, liver enzymes. My LDL went up, so I started a low-dose statin. My lymphocytes dipped a bit, so we lowered the dose. No shingles. No cancer. Just careful, consistent monitoring. It’s not perfect, but it’s working. I don’t see this as a danger-it’s a responsibility. And I’m glad my doctor treats it like one.
Arjun Deva
December 14, 2025 AT 21:18They’re lying. They’re ALL lying. The shingles rate? 23%? That’s a cover-up. The real number is 47%. The FDA doesn’t report the full data because they’re in bed with the drug companies. And the cholesterol? They call it ‘mild elevation’-but if your HDL drops and your triglycerides spike, you’re one heart attack away from a coroner’s report. And don’t forget-they’re already testing these drugs on children in clinical trials. Why? Because they want to make you dependent from birth. Wake up.
Mayur Panchamia
December 15, 2025 AT 23:12Listen here, folks-this isn’t medicine, it’s a corporate circus. JAK inhibitors? More like JAK-SCAM. They’re selling a placebo with side effects that look like a horror movie. And you know who’s laughing? The CEOs. They’re making billions while you’re stuck on statins, antivirals, and monthly blood tests. Meanwhile, real medicine-nutrition, movement, sleep-is ignored. Why? Because you can’t patent a kale smoothie. This isn’t progress-it’s exploitation dressed in white coats.
Kenny Pakade
December 17, 2025 AT 06:09So what? You think the FDA gives a damn about you? They approved this because it makes money. They don’t care if you get shingles or a heart attack-they care about quarterly earnings. And now you’re gonna sit there and say ‘monitoring’ fixes it? Monitoring doesn’t undo damage. It just lets them say ‘we warned you.’ I’d rather live with my arthritis than die from a pill that was never meant to heal me.
brenda olvera
December 18, 2025 AT 16:05I’ve seen people get their lives back with these drugs. My cousin had alopecia for 12 years-no hair, no confidence. Started ritlecitinib. Six months later, she had a full head of hair again. Yes, there are risks. But so is living in pain and shame. We don’t have to choose between fear and hope. We can be careful AND hopeful. Talk to your doctor. Get the labs. Take the antiviral. It’s not magic. But it’s worth it for some of us.
Clare Fox
December 18, 2025 AT 22:27i wonder if we’re treating the symptom or the story. what if the immune system isn’t ‘attacking’-but trying to tell us something? maybe the real fix isn’t blocking jaks, but listening to why the body went haywire in the first place. stress, diet, toxins, trauma… we just shove a pill in and call it a day. i’m not saying don’t use them. i’m saying don’t stop asking why.
Akash Takyar
December 19, 2025 AT 06:11As a physician in India, I have seen patients benefit immensely from JAK inhibitors when used appropriately. However, the lack of access to regular monitoring in low-resource settings is a serious concern. We must advocate for affordable lab kits, telemedicine follow-ups, and community health worker training to ensure safety. Innovation without equity is not progress-it is exclusion. Let us not replicate the mistakes of Western medicine by making these drugs available only to those who can afford the monitoring.
Nava Jothy
December 19, 2025 AT 07:18Oh, sweetie… you think this is the first time the pharmaceutical industry has sold you a fairy tale? *sips wine* JAK inhibitors? Please. They’re just the new OxyContin-with more blood tests and less addiction. You’re being groomed to believe that your body is broken and needs corporate chemistry to fix it. Meanwhile, your microbiome is screaming, your cortisol is through the roof, and your vitamin D is non-existent. But hey-at least your skin looks good, right? 😘