When your liver is struggling, food isn’t just fuel-it’s medicine. Many people think liver disease means cutting out alcohol and calling it a day. But if you have fatty liver, early-stage cirrhosis, or metabolic dysfunction-associated steatotic liver disease (MASLD), what you eat every day can actually reverse damage. The science is clear: a well-planned diet can lower liver enzymes by 20-30%, reduce liver fat by up to 40%, and even improve fibrosis scores without a single pill. This isn’t a fad. It’s the most effective, evidence-backed tool doctors now use to treat liver disease before it’s too late.
What a Liver-Healthy Diet Actually Looks Like
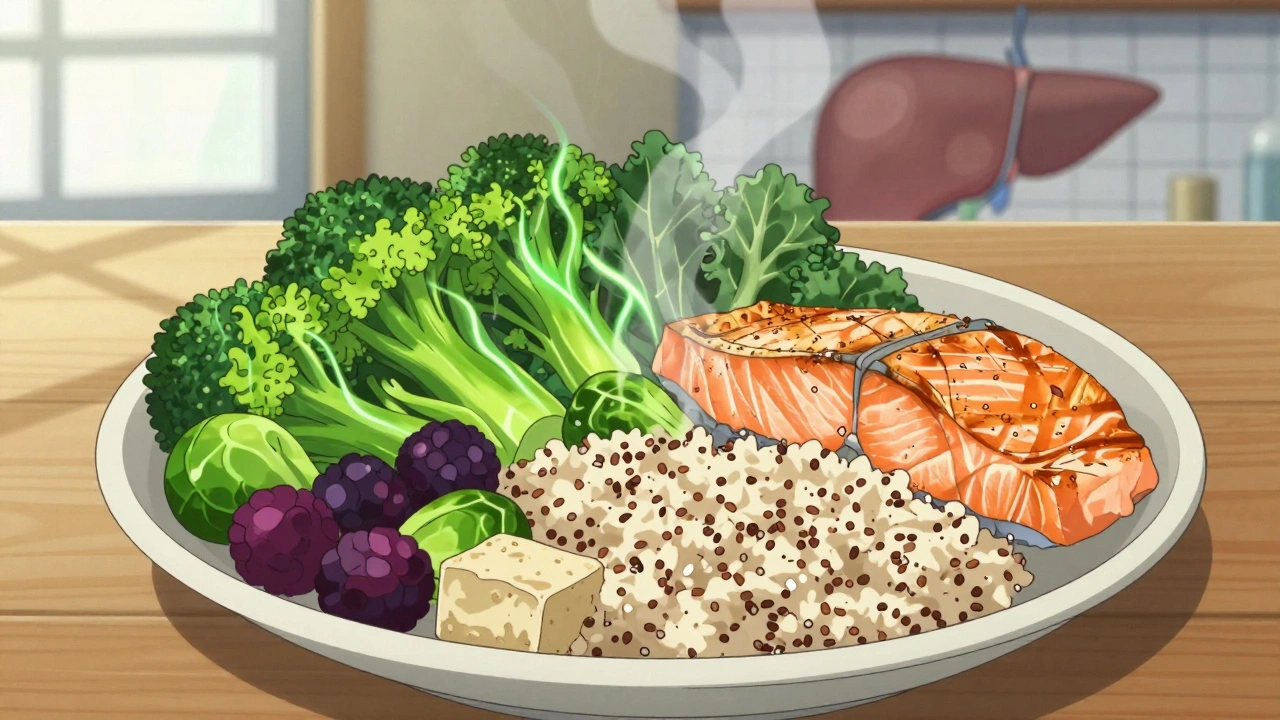
There’s no magic list of "liver superfoods." Instead, the best approach is a pattern-called the Mediterranean diet-that’s been tested in over 20 clinical trials and endorsed by the American Association for the Study of Liver Diseases (AASLD) and Mayo Clinic. This isn’t about deprivation. It’s about replacing the wrong foods with the right ones, consistently. Think of your plate this way: half filled with colorful vegetables and fruits. That’s not a suggestion-it’s a requirement. A 2023 study showed people who ate at least three servings of vegetables daily cut their liver fat by 18% in six months. Why? Cruciferous veggies like broccoli, kale, and Brussels sprouts contain compounds that help your liver detoxify harmful substances. Berries, especially blueberries and blackberries, are packed with anthocyanins. One trial found these antioxidants reduced liver inflammation by 25% in just 12 weeks. One-quarter of your plate should be lean protein. Not steak. Not fried chicken. Think fish like salmon or sardines, skinless chicken breast, tofu, or legumes. A 3-ounce portion-about the size of a deck of cards-is enough per meal. Too much protein can strain a damaged liver, but too little causes muscle loss, which makes liver disease worse. The sweet spot? 15-20% of your daily calories from protein. The last quarter? Whole grains. Brown rice, quinoa, oats, barley. These aren’t just "better than white bread." They’re fiber-rich, slow-digesting carbs that stabilize blood sugar and reduce fat buildup in the liver. The Mayo Clinic recommends getting 40-50% of your calories from these complex carbs. Avoid anything labeled "enriched" or "refined." Those are just sugar in disguise.What You Must Stop Eating
The biggest offenders aren’t hidden in some obscure snack aisle-they’re in your pantry, your fridge, and your daily coffee routine. First: sugary drinks. Soda, sweetened tea, fruit juice, energy drinks. One 12-ounce can has 39 grams of sugar-nearly 10 teaspoons. That sugar doesn’t go to your muscles. It goes straight to your liver, where it’s turned into fat. A 2022 review found that people who cut out sugary drinks lost 25-40% of their liver fat in six months, even without losing weight. Second: processed foods. Anything with a long ingredient list, especially if it includes "high-fructose corn syrup," "partially hydrogenated oils," or "modified starch." These foods spike insulin, promote fat storage in the liver, and trigger inflammation. A 2023 USDA analysis showed that switching from packaged meals to whole foods saved about $1.50 per meal-but more importantly, it cut liver fat markers significantly. Third: trans fats. Found in margarine, fried foods, and baked goods. These fats are proven to increase liver inflammation and oxidative stress. The FDA banned them in 2018, but they’re still lurking in some store-bought items. Always check the label: if it says "partially hydrogenated," put it back. And sodium. If you have advanced liver disease, too much salt causes fluid buildup in your belly and legs. Even if you don’t, aim for under 2,000 mg a day. That’s less than one teaspoon. Skip the soy sauce, canned soups, and deli meats. Flavor food with lemon, garlic, herbs, and vinegar instead.Why the Mediterranean Diet Wins Over Other Diets
You’ve probably heard of keto, low-fat, or intermittent fasting for liver health. Here’s the truth: none of them beat the Mediterranean diet. A 2021 meta-analysis compared 14 studies and found the Mediterranean diet reduced liver fat by 32% more than low-fat diets and 18% more than ketogenic diets. Why? Keto may burn fat quickly, but it often increases LDL cholesterol and puts stress on the liver. Low-fat diets often replace fat with sugar-worse than the original problem. The Mediterranean diet works because it’s balanced. It’s rich in monounsaturated fats from olive oil, nuts, and avocados. These fats lower bad cholesterol and reduce liver inflammation. A 2014 trial showed that replacing saturated fats with olive oil cut VLDL (a fat-carrying particle linked to fatty liver) by 30% in just eight weeks. The DASH diet, designed for high blood pressure, helps too-but it doesn’t focus on the anti-inflammatory fats and phytonutrients that directly target liver cells. Detox teas, juice cleanses, and liver "flushes"? They’re marketing gimmicks. The American Liver Foundation says there’s zero scientific evidence they help. Your liver detoxifies itself. All it needs is the right fuel.
Real People, Real Results
John M., 58, from Ohio, was diagnosed with stage 2 liver fibrosis. His FibroScan score was 12.5 kPa-indicating moderate scarring. His ALT (a liver enzyme) was 112 U/L (normal is under 40). He started the Mediterranean diet, walked 30 minutes daily, and cut out soda and processed snacks. Nine months later, his FibroScan dropped to 6.2 kPa. His ALT fell to 45. He didn’t lose 50 pounds. He didn’t take supplements. He just ate differently. On Reddit’s r/FattyLiver community, 68% of over 1,200 respondents said their energy improved within three months. But 42% said the hardest part was avoiding processed food because it was cheaper and easier. That’s real. A frozen bag of broccoli costs less than a box of chicken nuggets. A can of black beans is cheaper than a microwaveable meal. Planning ahead matters. Sarah K., who had migraines when she cut out all sugar, learned a key lesson: balance. Her doctor allowed 15 grams of natural sugar a day-mostly from berries. That’s about one cup of blueberries. It kept her headaches away and still helped her liver.How to Start Without Getting Overwhelmed
You don’t need to overhaul your life overnight. Start small. Step 1: Swap one drink. Replace your morning soda or sweet coffee with water, herbal tea, or sparkling water with lemon. That’s it. Do this for a week. Step 2: Add one vegetable to every meal. Spinach in your eggs. Carrots with your lunch. Broccoli with dinner. No recipe needed. Step 3: Cook one meal at home using whole ingredients. Try a simple recipe: grilled chicken, quinoa, roasted vegetables, and olive oil drizzle. Use frozen veggies if fresh are expensive or go bad too fast. Step 4: Read labels for hidden sugar. Look for words like: sucrose, dextrose, maltose, corn syrup, fruit juice concentrate. If sugar is listed in the top three ingredients, skip it. Step 5: Batch cook on Sunday. Cook a big pot of lentils, roast a tray of veggies, boil some eggs. Store them in the fridge. You’ll save time, money, and avoid temptation during the week. Most people find the first four weeks the hardest. After that, it becomes routine. The VCU School of Medicine found that 78% of new patients struggle with reading labels at first-but after six weeks, 92% could identify hidden sugars.What If You Can’t Afford Fresh Food?
Cost is a real barrier. But you don’t need organic kale or imported olive oil. Frozen vegetables are just as nutritious and often cheaper. Canned beans, lentils, and tuna in water are affordable protein sources. Oats, brown rice, and whole-wheat pasta are budget-friendly carbs. Eggs are one of the most affordable sources of high-quality protein. Harvard researchers ran community cooking classes in low-income neighborhoods. They taught people how to make Mediterranean-style meals using only supermarket staples. The result? A 35% drop in weekly food costs while improving liver markers. The VA Health System offers a free 12-week telehealth nutrition program for veterans with liver disease. Many state Medicaid plans now cover liver-specific diet counseling. Ask your doctor or call your local health department.
What About Supplements and Liver Cleanses?
Skip them. Milk thistle? Turmeric? Green tea extract? No study proves they reverse liver damage in humans. Some even harm the liver when taken in high doses. The only supplement with consistent evidence is vitamin E-but only for non-diabetic adults with confirmed NASH (a severe form of fatty liver). Even then, it’s used under medical supervision. Don’t self-prescribe. And no, a "liver cleanse" doesn’t work. Your liver doesn’t need flushing. It needs rest. And the best way to give it rest is to stop flooding it with sugar, alcohol, and toxins.When Diet Isn’t Enough
Diet is the first and most powerful tool-but not the only one. If you have advanced cirrhosis, your doctor may need to limit protein temporarily to prevent confusion or brain fog (hepatic encephalopathy). But this is rare and temporary. Most people need more protein, not less, to prevent muscle wasting. Weight loss helps. Losing just 5-7% of your body weight can reduce liver fat. But you don’t need to lose 50 pounds to see improvement. Even small changes in diet improve liver enzymes. Exercise matters too. Walking 150 minutes a week (about 30 minutes, five days a week) improves liver health independently of weight loss. Combine movement with diet, and results multiply.The Future of Liver Nutrition
Science is moving fast. Researchers at Mayo Clinic are now studying how your gut bacteria predict which foods will work best for your liver. One person might respond to walnuts. Another to blueberries. Personalized nutrition for liver disease is coming-and it’s already being tested in clinical trials. The European Association for the Study of the Liver is running a major trial testing time-restricted eating: eating all meals within a 10-hour window. Early results show a 27% greater drop in liver fat than diet alone. By 2030, doctors may track your dietary adherence as closely as they track your ALT levels. Because the data is undeniable: what you eat determines how your liver heals.Can a liver-healthy diet reverse fatty liver disease?
Yes, especially in early stages. Studies show that following a Mediterranean-style diet can reduce liver fat by 25-40% and lower liver enzymes by 20-30% within 6-12 months. Even without weight loss, dietary changes improve liver health. The key is consistency-replacing sugar, processed foods, and unhealthy fats with vegetables, whole grains, lean protein, and healthy fats.
Is the keto diet good for the liver?
Not ideal. While keto can cause rapid fat loss, it often increases LDL cholesterol and may raise liver stress due to high saturated fat intake. A 2021 meta-analysis found the Mediterranean diet reduced liver fat 18% more than ketogenic diets after 12 months. Keto might help short-term, but it’s not sustainable or as effective for long-term liver healing.
How much sugar is safe for someone with liver disease?
Aim for less than 10% of your daily calories from added sugar-that’s about 25 grams (6 teaspoons) for a 2,000-calorie diet. Avoid sugary drinks completely. Natural sugars from whole fruits (like berries, apples, oranges) are fine in moderation-up to 2-3 servings per day. The problem isn’t fruit; it’s juice, soda, and processed snacks loaded with high-fructose corn syrup.
Do I need to avoid all fats if I have fatty liver?
No-avoid the wrong fats. Saturated fats (fried foods, butter, fatty meats) and trans fats (margarine, packaged snacks) are harmful. But healthy fats like olive oil, avocado, nuts, and fatty fish (salmon, sardines) are essential. They reduce inflammation and help your liver repair. Aim for 40% of your fat intake to come from monounsaturated fats like olive oil.
Can I drink alcohol with a fatty liver?
No. Even small amounts of alcohol can worsen liver damage in people with fatty liver disease. The liver prioritizes breaking down alcohol over fat, which increases fat buildup. For best results, avoid alcohol completely. If you have cirrhosis, any alcohol is dangerous and can be life-threatening.
How long does it take to see results from a liver-healthy diet?
Most people notice improved energy and less bloating within 2-4 weeks. Blood tests (like ALT and AST) often improve within 3 months. Liver fat reduction shows up on scans after 6-12 months. The key is sticking with it. Even small, consistent changes add up over time.
Are there any foods that specifically heal the liver?
No single food heals the liver. But certain foods support its function: walnuts (30g/day reduce bad cholesterol), cruciferous vegetables (broccoli, kale), berries (anthocyanins reduce inflammation), coffee (linked to lower liver fibrosis), and green tea (antioxidants). The best approach is variety-eat a rainbow of whole foods daily.
Can I eat out on a liver-healthy diet?
Yes, but be strategic. Choose grilled or baked proteins, ask for steamed or roasted vegetables, and request whole grains. Skip sauces, dressings, and fried sides. Ask for olive oil and vinegar instead of butter or creamy dressings. Avoid sugary drinks and desserts. Most restaurants can accommodate these requests-you just need to ask.

Alexander Williams
December 2, 2025 AT 12:37The Mediterranean diet isn't some revolutionary breakthrough-it's just a rebranding of what our grandparents ate before corporations turned food into a pharmacological experiment. The real data? Most clinical trials are funded by olive oil conglomerates or agribusinesses pushing plant-based agendas. And let's not pretend fiber magically detoxifies the liver-it's just a placebo effect wrapped in peer-reviewed jargon. The liver doesn't need "fuel." It needs to be left alone. Fasting, not food, is the true hepatoprotective intervention.
Also, why is no one talking about glyphosate? The USDA's own data shows it accumulates in hepatic tissue. But you won't hear that from Mayo Clinic-they're too busy endorsing salad bowls funded by Big Organic.
TL;DR: Eat less. Move less. Stop believing in food as therapy.
Suzanne Mollaneda Padin
December 3, 2025 AT 12:25I’ve been following this protocol for 14 months after my ALT hit 150. The changes weren’t dramatic at first, but by month 6, my energy was up, brain fog lifted, and my doctor was stunned at the FibroScan drop. I didn’t lose weight-I just swapped soda for sparkling water, ate more lentils, and stopped buying anything with more than 5 ingredients.
My mom in Manila still cooks me batches of brown rice and steamed fish every month. She says, "Food is love, not punishment." And she’s right. It’s not about restriction. It’s about returning to what nourishes, not just fills.
For anyone overwhelmed: start with one veggie at dinner. That’s it. You don’t need a spreadsheet. You need consistency. And maybe a little help from someone who cares.
Bonnie Youn
December 4, 2025 AT 03:54YESSSS this is the truth I’ve been screaming into the void for years
My liver enzymes were through the roof and I thought I needed some miracle supplement or detox tea or whatever
Turns out I just needed to stop drinking Mountain Dew like it was water and eat broccoli with my eggs
3 months later I feel like a new person and my husband says I don’t yell as much which is a miracle
Stop overcomplicating it. Food is medicine. Not a cult. Not a trend. Just eat real stuff. Period.
Also frozen veggies are your best friend. No shame. I use them every damn day.
Edward Hyde
December 5, 2025 AT 09:18Oh wow. Another sanctimonious food blog masquerading as science. Let me guess-you also think kale cures cancer and that your kombucha is a spiritual cleanse?
The entire premise is bullshit. The liver doesn’t care if you eat quinoa or white rice. It cares if you’re insulin resistant, sedentary, and chronically stressed. You’re blaming food because it’s easier than admitting your life is a dumpster fire.
And don’t get me started on the olive oil cult. That stuff oxidizes in your kitchen if you leave the cap off. You’re literally feeding your liver rancid fat.
Go lift weights. Sleep 7 hours. Stop eating at 8 PM. That’s the real protocol. The rest is influencer noise.
Margaret Stearns
December 6, 2025 AT 22:18i started doing the swap one drink thing and it actually worked
i used to have 2 sugary coffees a day and now i just have black coffee with a splash of almond milk
my stomach stopped bloating after 2 weeks
also i bought frozen broccoli and threw it on everything
no fancy recipes
just more veggies less stuff in packages
its not perfect but its better
thank you for writing this
Scotia Corley
December 7, 2025 AT 11:48While the dietary recommendations presented are broadly consistent with current clinical guidelines, the underlying assumption-that nutritional intervention alone can reverse fibrotic progression-remains empirically unsupported in advanced cases. The referenced 2023 study on cruciferous vegetables lacks control for confounding variables including caloric intake, physical activity, and genetic predisposition.
Moreover, the assertion that "the liver detoxifies itself" is a semantic misrepresentation. Hepatic detoxification is a metabolically expensive process requiring cofactors such as glutathione, taurine, and adequate protein. Depriving the system of these substrates while advocating for "whole foods" is physiologically incoherent.
This article, while well-intentioned, dangerously oversimplifies a complex hepatometabolic disorder. The emphasis on affordability and convenience is commendable, yet it neglects the role of epigenetic regulation and gut-liver axis modulation. A more rigorous approach would integrate microbiome profiling and metabolic phenotyping.
Karandeep Singh
December 9, 2025 AT 06:21india here
we eat dal rice roti
no olive oil
no quinoa
but our liver is fine
because we dont drink soda
and we dont eat chips
simple
Mary Ngo
December 9, 2025 AT 18:52Have you considered that this entire "liver diet" narrative is a distraction orchestrated by Big Pharma to keep us focused on food while they quietly patent synthetic liver regenerators?
The FDA banned trans fats in 2018-but did you know that the same year, they approved a new class of hepatotoxic antidiabetics? Coincidence? Or a controlled release of dietary misinformation to mask the real toxicity?
They want you to believe you can eat your way out of a systemic metabolic collapse. But the truth? Your liver is a canary in the coal mine for a poisoned ecosystem. Glyphosate, PFAS, microplastics-they’re in your water, your salt, your air. No amount of broccoli will neutralize that.
And yet, here we are, debating spinach over supplements. How convenient.
Wake up. The real cleanse isn’t in your fridge. It’s in your protest.
They don’t want you to heal. They want you to consume better.