Edema Medication Selection Guide
Select Your Condition
Treatment Recommendations
Select your condition and enter your patient's information to see treatment recommendations.
Key Takeaways
- Diuretics are the first‑line meds for most types of edema, but several non‑diuretic options can improve outcomes.
- Choosing a drug depends on the edema cause, kidney function, and electrolyte profile.
- Loop diuretics work fastest; thiazides are milder; potassium‑sparing agents protect against low potassium.
- Newer classes like SGLT2 inhibitors and vasodilators treat fluid overload in heart‑failure or kidney disease without classic diuretic mechanisms.
- Close monitoring of weight, blood pressure, and labs reduces the risk of complications.
When fluid builds up in tissues, edema is the swelling caused by excess interstitial fluid, often signaling underlying health issues such as heart failure, kidney disease, liver cirrhosis, or medication side effects. Managing this swelling isn’t just about squeezing a pillow; it’s about targeting the underlying cause with the right medication, lifestyle tweaks, and regular check‑ins. Below we break down how diuretics work, what alternatives exist, and how to stitch everything together into a safe, effective plan.
What Is Edema and Why Does It Require Medication?
Edema can appear in the legs, abdomen, lungs, or even the brain. In mild cases, a simple elevation of the legs may help, but when the fluid volume is high or the cause is chronic, doctors turn to drugs to shift water out of the interstitial space and into the kidneys for excretion.
Key questions clinicians ask before prescribing:
- Is the swelling pitting (leaves a dent) or non‑pitting?
- What organ system is driving the fluid buildup?
- What is the patient’s baseline kidney function (eGFR) and electrolyte balance?
Answers guide whether a diuretic is appropriate or if a non‑diuretic approach is safer.
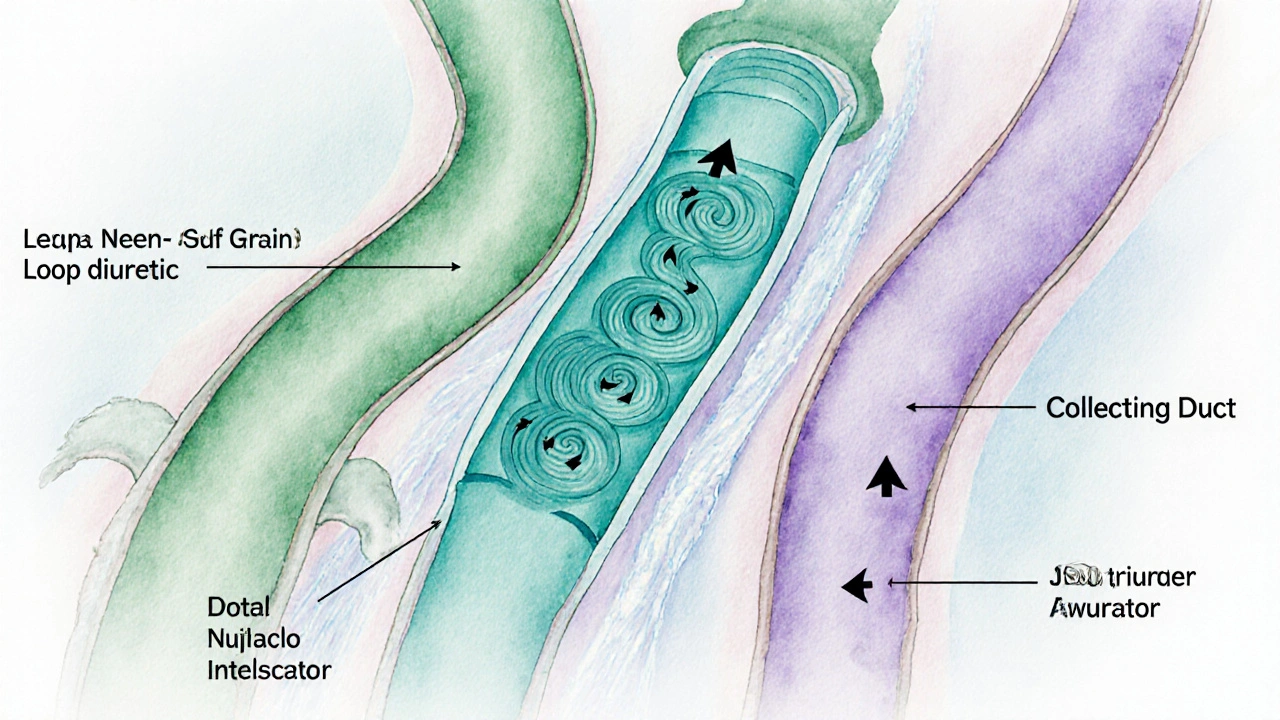
How Diuretics Work: The Core Mechanism
Diuretics are medications that increase urine output by altering sodium and water reabsorption in different parts of the nephron. By forcing the kidneys to excrete more sodium, water follows, reducing plasma volume and, ultimately, interstitial fluid.
Three main sites of action explain why some diuretics act faster or stronger than others:
- The loop of Henle - high‑capacity site, fast and powerful fluid removal.
- The distal convoluted tubule - moderate capacity, useful for chronic management.
- The collecting duct - fine‑tuning of potassium and sodium balance.
Understanding these sites helps match the drug to the patient’s needs.
Common Diuretic Classes
Loop Diuretics
Loop diuretics (e.g., furosemide, bumetanide, torsemide) block the Na‑K‑2Cl co‑transporter in the thick ascending limb. They can increase urine output by up to 30mL per hour, making them the go‑to for急急急急急急急急急急急急急急急急急急急急急急急急急urgent‑onset edema such as pulmonary congestion in heart failure.
Typical starting dose: furosemide 20-40mg orally once daily; titrate based on weight loss (≈1kg per 40mg). Monitor potassium, magnesium, and creatinine within 48hours.
Thiazide Diuretics
Thiazide diuretics (hydrochlorothiazide, chlorthalidone) inhibit the Na‑Cl transporter in the distal convoluted tubule. They’re milder (≈10mL per hour) but excellent for chronic peripheral edema and hypertension.
Starting dose: hydrochlorothiazide 12.5mg daily. Watch for hyponatremia, especially in older adults.
Potassium‑Sparing Diuretics
Aldosterone antagonists such as spironolactone or eplerenone act on the collecting duct, reducing sodium reabsorption while keeping potassium. They’re often added to loop therapy to blunt potassium loss.
Spironolactone 25mg daily can reduce edema and improve mortality in systolic heart failure. Check potassium before each dose; keep serum K⁺ between 4.0-5.0mmol/L.
Combined Strategies
Many patients benefit from a loop + potassium‑sparing combo, especially when high doses of loops cause hypokalemia. The key is balanced monitoring.
Beyond Classic Diuretics: Emerging and Adjunct Options
SGLT2 Inhibitors
SGLT2 inhibitors (dapagliflozin, empagliflozin) were designed for diabetes but also promote glycosuric osmotic diuresis, lowering plasma volume. Trials in 2023‑2024 showed a 30% reduction in heart‑failure hospitalizations, even in non‑diabetic patients.
Typical dose: dapagliflozin 10mg once daily. Monitor for genital infections and volume depletion.
Vasodilators & Afterload Reducers
Agents such as hydralazine or nitrates lower systemic vascular resistance, indirectly reducing capillary hydrostatic pressure and fluid leakage. They’re useful when edema stems from high afterload (e.g., severe aortic stenosis) rather than volume excess.
ACE Inhibitors & ARBs
These drugs improve renal perfusion and blunt the renin‑angiotensin‑aldosterone system, curbing sodium retention. In chronic kidney disease, low‑dose lisinopril (5mg) can shrink leg swelling over weeks.
Albumin Infusions
In hypo‑albuminemic states (nephrotic syndrome, severe liver disease), raising oncotic pressure with albumin can pull fluid back into vessels. It’s a short‑term bridge, not a long‑term edema cure.
Choosing the Right Regimen: A Practical Framework
Use this step‑by‑step checklist to decide:
- Identify the cause. Heart failure → consider loop + SGLT2; liver cirrhosis → combine diuretic with albumin.
- Assess kidney function. eGFR>30mL/min/1.73m² allows loops; eGFR<30 may require thiazide‑sparing combos or non‑diuretic agents.
- Check electrolytes. Low potassium → add aldosterone antagonist; high sodium → reduce dietary intake.
- Start low, go slow. Begin with the weakest effective dose, titrate every 3‑5days based on weight change (aim≈0.5-1kg per day) and symptom relief.
- Monitor. Weight, blood pressure, serum creatinine, and potassium at baseline, 48h, then weekly for the first month.
For patients with resistant edema, consider combining a loop with an SGLT2 inhibitor plus an aldosterone antagonist-an evidence‑based “triple‑hit” strategy shown to cut rehospitalization rates by 20% in a 2024 multicenter trial.
Managing Side Effects & Safety Tips
Diuretic‑related issues are common but manageable:
- Hypokalemia: Eat bananas, potatoes, or add a potassium‑sparing agent.
- Hyponatremia: Reduce free water intake; consider a thiazide‑sparing approach.
- Renal function decline: Pause or halve the dose if creatinine rises >0.3mg/dL in 48h.
- OTC interactions: NSAIDs blunt diuretic efficacy and raise kidney risk-advise patients to avoid regular ibuprofen.
Educate patients to report dizziness, rapid weight loss (>2kg/day), or muscle cramps immediately.

Lifestyle & Adjunct Measures That Complement Meds
Medication alone rarely solves edema. Pair drugs with these practical steps:
- Fluid restriction: 1.5-2L/day for heart‑failure patients; avoid sugary drinks.
- Low‑salt diet: <5g of sodium per day (~2g of salt) reduces the workload on diuretics.
- Compression stockings: Class2 (23‑32mmHg) stockings improve venous return in chronic leg edema.
- Regular ambulation: Walking 30minutes daily mobilizes fluid from the legs back to the core.
These measures can shrink the required diuretic dose, lowering the risk of side effects.
Quick Reference Table: Diuretics vs. Non‑Diuretic Options
| Agent | Primary Site | Typical Indication | Onset (hrs) | Major Side‑effects |
|---|---|---|---|---|
| Loop diuretic (furosemide) | Thick ascending limb | Acute heart‑failure, pulmonary edema | 0.5‑2 | Hypokalemia, ototoxicity at high doses |
| Thiazide (hydrochlorothiazide) | Distal convoluted tubule | Chronic peripheral edema, hypertension | 4‑6 | Hyponatremia, hyperuricemia |
| Aldosterone antagonist (spironolactone) | Collecting duct | Heart‑failure, cirrhosis | 6‑12 | Hyperkalemia, gynecomastia |
| SGLT2 inhibitor (dapagliflozin) | Proximal tubule (glucose‑SGLT2) | Heart‑failure (with/without diabetes) | 12‑24 | Genital infections, volume depletion |
| Vasodilator (hydralazine) | Arterial smooth muscle | High afterload, refractory edema | 1‑2 | Reflex tachycardia, headache |
Mini FAQ
Frequently Asked Questions
Can I stop diuretics once my legs look better?
Stopping abruptly can cause fluid rebound. Taper the dose gradually while monitoring weight and blood pressure. Your doctor should guide the schedule.
Are SGLT2 inhibitors safe for non‑diabetic patients?
Yes. Recent heart‑failure trials enrolled patients without diabetes and showed similar benefits. Kidney function must be ≥30mL/min/1.73m², and patients should stay hydrated.
Why does my doctor avoid NSAIDs while I’m on diuretics?
NSAIDs constrict afferent arterioles in the kidney, reducing the diuretic’s ability to excrete sodium and raising the risk of acute kidney injury.
What is a safe rate of weight loss when using diuretics?
Aim for 0.5-1kg per day (about 1-2pounds). Faster loss may signal over‑diuresis, leading to low blood pressure or electrolyte disturbances.
Do compression stockings replace medication?
They help with venous pooling but don’t address the underlying fluid overload. Use them alongside meds for best results.
Understanding the pharmacology, knowing when to add newer agents, and staying vigilant with labs makes edema treatment far less of a guessing game. With the right mix of drugs, diet, and monitoring, most patients can reclaim mobility and comfort without constant hospital visits.


Kai Röder
October 12, 2025 AT 06:14Thanks for putting together such a thorough guide. The breakdown of diuretic classes really helps clinicians quickly decide which drug to start with. I also appreciate the practical checklist at the end – it’s the kind of tool that can be printed and kept at the bedside. Remember to tailor the dose based on patient weight and renal function, as you mentioned. Keep up the good work!
Brandi Thompson
October 18, 2025 AT 14:47Wow this article really dives deep into the whole world of edema treatments and I have to say it feels like you’ve covered every angle from loops to SGLT2 inhibitors and even the nitty gritty of potassium monitoring I think the detail is admirable but honestly the way it’s written sometimes feels like a lecture that never ends it’s as if each paragraph is trying to outdo the previous one in length and complexity and while that can be impressive it also makes it hard for a busy practitioner to skim for the key points the endless list of drug names and dosage ranges can be overwhelming especially when you’re dealing with a patient in the ER who needs immediate decisions I get that you want to be thorough but maybe a quick reference table would have helped a lot also the repeated warnings about NSAIDs feel a bit redundant after the first mention still the article does a solid job of tying together the pathophysiology and the pharmacology and for anyone who really wants to understand the why behind each choice this is a gold mine thanks for the effort
Chip Hutchison
October 24, 2025 AT 23:21I love how you laid out the step‑by‑step framework; it makes it feel approachable. The inclusion of both lab values and medication interactions is especially useful for trainees. It’s also nice to see lifestyle tips woven in – we often forget those basics. One suggestion: a quick FAQ at the bottom could address common pitfalls. Overall, great job making a complex topic digestible.
Emily Moody
October 31, 2025 AT 06:54This piece reads like a manifesto for modern heart‑failure management – bold, data‑driven, and unapologetically clinical. The jargon‑heavy sections on SGLT2 mechanisms could scare off the lay reader, but the target audience will appreciate the depth. Your dramatic flair when describing volume overload really pumps the adrenaline. Keep the color, but maybe tone down the hype a notch.
Prateek Kohli
November 6, 2025 AT 15:27Nice work! The balanced tone makes it easy to follow 😊 The emoticon adds a friendly touch.
Noah Seidman
November 13, 2025 AT 00:01While the guide is comprehensive, I can’t help but question the ethical implications of blanket prescribing loops without emphasizing patient autonomy. Philosophically, medicine should empower patients, not just dump diuretics. Your protocol seems to prioritize efficiency over individualized care. A contrarian view: perhaps we need more shared decision‑making tools embedded.
Anastasia Petryankina
November 19, 2025 AT 08:34Oh, look, another “definitive” guide that pretends to be the final word. How original. I guess we’ll all just nod and move on.
Zane Nelson
November 25, 2025 AT 17:07The article is thorough, albeit a tad pedantic. One could argue it borders on over‑analysis.
Sahithi Bhasyam
December 2, 2025 AT 01:41The guide, overall, is well‑structured, comprehensive, and very helpful, however, there are some minor typos, like "急急急急急急急急急急急急急急急急急急急急急急急急急" which could be cleaned up, and the use of commas could be more consistent!!! ;)
Kayla Reeves
December 8, 2025 AT 10:14Honestly, this reads like a checklist for the uninspired. Minimal insight, just regurgitated guidelines. Not impressed.
Abhinanda Mallick
December 14, 2025 AT 18:47Well, if you’re looking for a theatrical performance of renal physiology, this is it – the drama of electrolytes, the crescendo of diuretic action! Yet, the jargon occasionally drags like a bad soap opera script. The emotional undertones are palpable, especially when warning about NSAIDs. Still, the core advice is solid, even if delivered with melodramatic flair.
Richard Wieland
December 21, 2025 AT 03:21Concise and clear, the guide hits the philosophical heart of why we treat edema. Simplicity is a virtue.
rachel mamuad
December 27, 2025 AT 11:54I r e al ly like the depth of the pharmacology part, but some parts of the text have mispellings like "culturual" and "recomended" that could be fixed. Also the use of medical lingo is good but might alienate non‑clinicians. Overall a solid piece, just polish the edges.
Maricia Harris
January 2, 2026 AT 20:27Another "expert" guide that pretends to be novel. Honestly, it feels like a rehash of old lectures. The drama is missing, so where’s the entertainment?
Tara Timlin
January 9, 2026 AT 05:01Great summary!