When your waistline grows, your triglycerides climb, and your blood sugar starts creeping up, it’s not just about looking different or feeling a little sluggish. These aren’t separate issues-they’re signs of the same hidden problem: metabolic syndrome. This isn’t a disease you can point to on a chart. It’s a cluster of warning signs that your body’s metabolism is falling apart. And if left unchecked, it sets the stage for heart attacks, strokes, and type 2 diabetes.
What Exactly Is Metabolic Syndrome?
Metabolic syndrome isn’t one thing. It’s three or more of five specific problems happening at once. The most important of these? Your waist size. If you’re a man with a waist over 40 inches (102 cm), or a woman with a waist over 35 inches (88 cm), that’s the red flag that starts the whole chain reaction. This isn’t about being overweight-it’s about fat gathering deep inside your belly, around your liver and organs. That’s visceral fat, and it’s metabolically active. It doesn’t just sit there. It sends out chemicals that mess with how your body uses insulin. The other four signs? High triglycerides (150 mg/dL or more), low HDL cholesterol (under 40 for men, under 50 for women), high blood pressure (130/85 or higher), and fasting blood sugar of 100 mg/dL or more. You don’t need all five. Just three. And if you have them, your risk of heart disease doubles. Your chance of developing type 2 diabetes goes up fivefold.Why Waist Size Is the Trigger
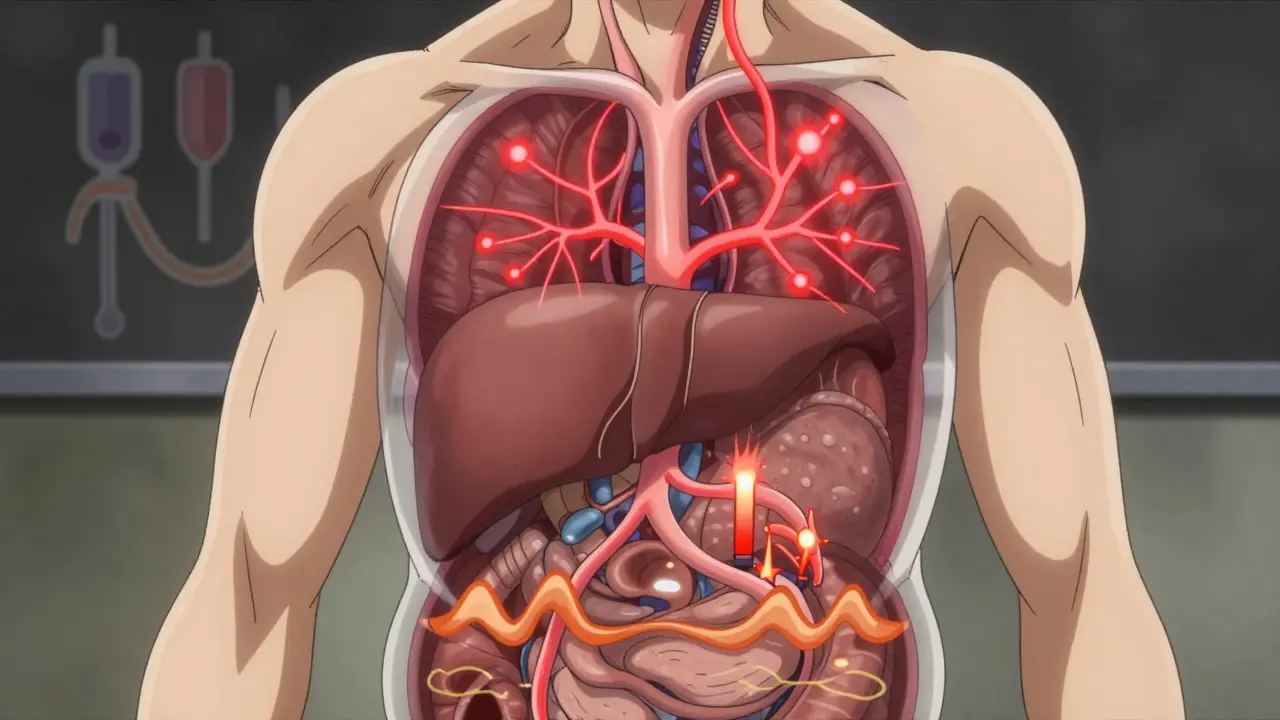
Think of your belly fat like a faulty factory. When it gets too big, it starts leaking harmful substances-like tumor necrosis factor-alpha and resistin-into your bloodstream. These chemicals make your muscles, liver, and fat cells blind to insulin. Insulin is the key that lets sugar into your cells for energy. When it doesn’t work, sugar stays in your blood. That’s high glucose. And your liver, trying to compensate, starts making more fat-triglycerides-and pumping them into your blood. This isn’t theoretical. Research from Washington University showed that people with high waist measurements had fatty acids flooding their liver, directly causing triglyceride levels to rise. And those same fatty acids made their muscles even less responsive to insulin. It’s a loop: more belly fat → worse insulin resistance → higher triglycerides → higher blood sugar → even more fat storage. The numbers don’t lie. Every extra 4 inches (10 cm) around your waist increases your risk of heart disease by 10%, even if your BMI is normal. That’s why two people with the same weight can have wildly different risks-one with fat spread out, the other with a thick waistline. The one with the bigger waist? That’s the one heading toward metabolic syndrome.Triglycerides: More Than Just a Number
Triglycerides are the main form of fat in your blood. When you eat more calories than you burn, your body turns the extra into triglycerides and stores them. But with metabolic syndrome, your body isn’t just storing fat-it’s overproducing it. Levels above 150 mg/dL count as a diagnostic marker. But here’s what most people don’t know: once you hit 200 mg/dL, your risk of heart disease jumps independently of your LDL (the so-called “bad” cholesterol). That’s because high triglycerides are linked to smaller, stickier LDL particles that clog arteries more easily. They also lower HDL (the “good” cholesterol), which normally helps clean up plaque. And it’s not just diet. Alcohol, sugary drinks, and refined carbs like white bread and pastries are major drivers. A single 20-ounce soda can spike triglycerides by 30% in healthy people-and even more if you already have insulin resistance. The American Heart Association says limiting added sugar to under 10% of your daily calories and keeping alcohol to one drink a day (for women) or two (for men) is critical.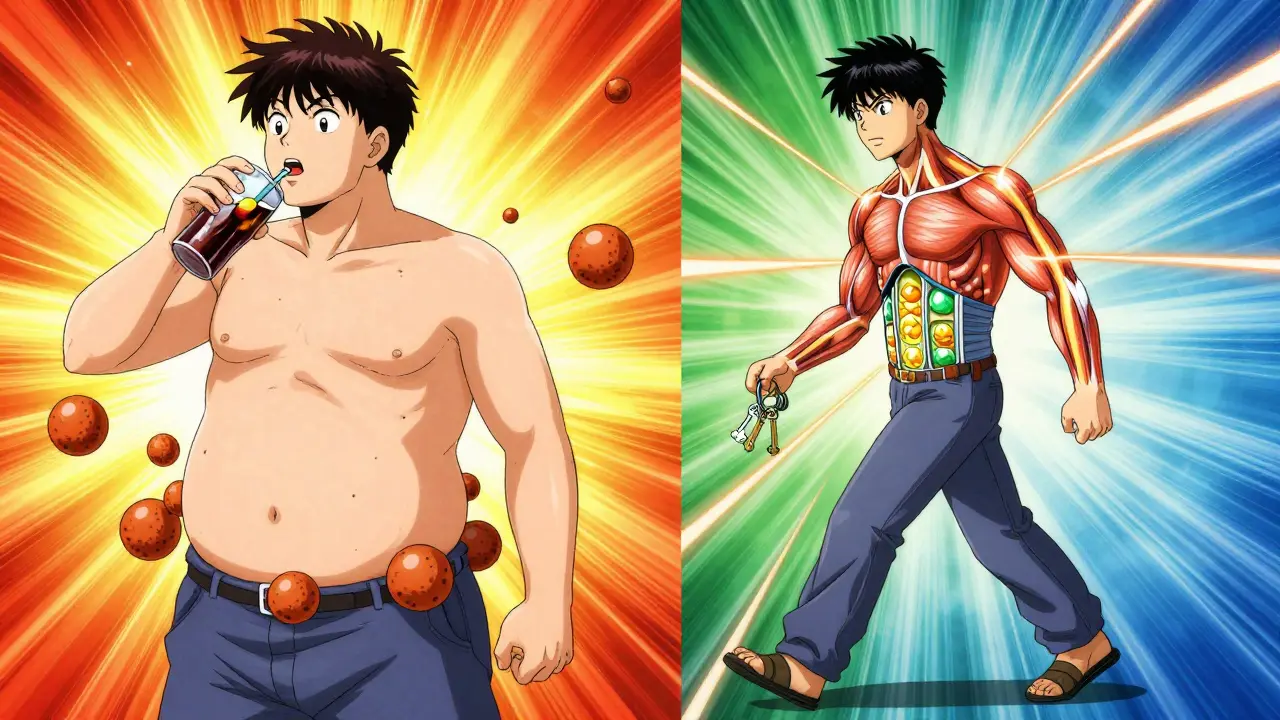
Glucose Control: The Silent Breakdown
Fasting blood sugar of 100 mg/dL or higher is the marker for prediabetes. But this isn’t just about sugar. It’s about your body’s ability to handle it. When your cells stop responding to insulin, your pancreas pumps out more and more to compensate. That’s called hyperinsulinemia. It’s your body’s last-ditch effort to keep glucose down. But eventually, the pancreas gets tired. Insulin production drops. Blood sugar rises. And that’s when prediabetes becomes type 2 diabetes. The Diabetes Prevention Program showed that people with fasting glucose between 100-125 mg/dL had a 5-10% chance each year of turning diabetic-unless they changed their habits. The good news? Lifestyle changes can reverse this. Losing just 5-10% of your body weight can bring glucose levels back into the normal range. Eating more fiber, cutting out sugary drinks, and moving more helps your cells become sensitive to insulin again. In fact, intensive lifestyle changes reduced diabetes risk by 58% over three years-more than any drug.The Connection: Insulin Resistance Is the Core
All three-waist size, triglycerides, and glucose-are tied together by one root cause: insulin resistance. That’s the missing link most doctors still overlook. You can have high triglycerides without insulin resistance. You can have high blood sugar without belly fat. But when you have all three? Insulin resistance is the engine driving them. Dr. Robert Eckel, who helped write the official guidelines, calls abdominal obesity the “trigger.” Once fat builds up around your organs, it sets off inflammation and hormonal chaos. Your liver starts making more triglycerides. Your muscles stop taking in glucose. Your blood pressure rises because insulin affects kidney function. It’s all connected. That’s why treating just one part doesn’t work. Taking a statin for cholesterol won’t fix your blood sugar. Taking metformin for glucose won’t shrink your waist. You have to tackle the whole system.What You Can Do: Real Steps That Work
The good news? Metabolic syndrome isn’t a life sentence. It’s reversible. And the most powerful tool? Weight loss through lifestyle change.- Move more. Aim for at least 150 minutes a week of brisk walking, cycling, or swimming. Studies show that even short walks after meals help lower blood sugar spikes.
- Eat differently. Swap out processed carbs for vegetables, legumes, whole grains, nuts, and lean proteins. The Mediterranean diet has been proven to cut heart events by 30% in high-risk people. It’s not about restriction-it’s about real food.
- Drop the sugar. Read labels. Avoid high-fructose corn syrup, sodas, sweetened coffee, and fruit juices. Sugar is the main fuel for liver fat and triglyceride production.
- Limit alcohol. One drink a day for women, two for men. More than that? It directly raises triglycerides and worsens insulin resistance.
- Sleep and stress matter. Poor sleep and chronic stress raise cortisol, which increases belly fat and blood sugar. Aim for 7-8 hours a night. Try breathing exercises or walks in nature.

When Medication Might Help
Lifestyle is the foundation. But sometimes, you need backup. If your triglycerides are above 500 mg/dL, your doctor may prescribe omega-3 fatty acids. If your blood sugar stays high despite changes, metformin is often used-it improves insulin sensitivity and can even help with weight loss. Blood pressure meds like ACE inhibitors may be added if your pressure won’t budge. But here’s the catch: drugs don’t fix the root. They manage symptoms. Only losing weight, moving more, and eating better can reverse insulin resistance. The National Heart, Lung, and Blood Institute says weight loss is the single most effective strategy for reversing all five components of metabolic syndrome.What’s Next: New Tools and Hope
Science is moving fast. Researchers now use something called the TyG index-calculated from your fasting triglycerides and glucose-to estimate insulin resistance without expensive tests. Some are even looking at gut bacteria as a potential target for treatment. And in 2024, the American Diabetes Association introduced a new “metabolic health” score that includes continuous glucose monitoring data. This means we’re moving beyond single numbers. We’re looking at patterns-how your body responds to food, movement, and sleep over time. The big picture? By 2030, half of adults in developed countries may have metabolic syndrome. But it doesn’t have to be that way. The tools to reverse it are simple, proven, and available now. It’s not about perfection. It’s about progress. Start with one change: cut out sugary drinks. Walk for 20 minutes after dinner. Measure your waist once a month. Small steps, done consistently, can turn a dangerous cluster of numbers into a story of recovery.Can you have metabolic syndrome without being overweight?
Yes. While belly fat is the main driver, some people-especially those of South Asian, Hispanic, or Indigenous descent-develop metabolic syndrome at lower body weights. Their bodies store fat more easily around organs, even if they look thin. That’s why waist size matters more than BMI. A person with a normal BMI but a waist over 35 inches (women) or 40 inches (men) can still meet the criteria.
Does metabolic syndrome always lead to diabetes?
No, but the risk is very high. About 50% of people with metabolic syndrome will develop type 2 diabetes within 10 years if nothing changes. But studies show that losing just 5-7% of body weight and getting 150 minutes of exercise a week cuts that risk by more than half. It’s preventable-but only if you act.
Can medications cure metabolic syndrome?
No. Medications like metformin, statins, or blood pressure pills help manage individual parts of metabolic syndrome, but they don’t reverse the root cause: insulin resistance. Only weight loss, better food choices, and regular movement can do that. Drugs are support tools, not solutions.
How often should I check my waist, triglycerides, and blood sugar?
If you’re at risk-over 40, have a family history of diabetes or heart disease, or carry extra weight around your middle-get checked yearly. If you’ve been diagnosed with metabolic syndrome, check your waist every 1-2 months to track progress. Blood tests for triglycerides and glucose should be done every 3-6 months until levels improve, then annually. Home glucose monitors can help if you’re prediabetic.
Is metabolic syndrome the same as diabetes?
No. Metabolic syndrome is a group of risk factors that make diabetes and heart disease much more likely. Diabetes is when your blood sugar is consistently high due to insulin failure. Metabolic syndrome is the warning sign that you’re on the path to diabetes-if you don’t change course. Think of it as the red zone before the crash.

Kayleigh Campbell
December 15, 2025 AT 09:28So let me get this straight - your belly fat is basically a tiny, angry factory dumping poison into your bloodstream? And we’re supposed to just blame ourselves for having a waistline? Cool. I’ll just stop breathing while I’m at it, since lungs also produce CO2. This isn’t science, it’s a guilt trip with graphs.
But hey, if cutting out soda and walking after dinner fixes everything, why does Big Pharma still make billions? Just saying.
Also, ‘metabolic syndrome’ sounds like a Netflix documentary about a broken toaster. We need better branding.
Still… I did swap my morning orange juice for black coffee. And my waistband feels looser. So maybe… just maybe… there’s something here.
Not buying the hype. But buying the spinach.
Dave Alponvyr
December 15, 2025 AT 16:29Waist size > BMI. That’s the only thing you need to remember.
Stop weighing yourself. Start measuring your waist.
Do it today.
Cassandra Collins
December 16, 2025 AT 18:07Okay but have you heard about the 2023 CDC leak? They admitted that waist measurements were manipulated to push statins and metformin. The real cause? 5G towers and fluoride in the water. I measured my waist after a 3-day juice cleanse and it went UP. Coincidence? I think not.
Also, my neighbor’s cat got metabolic syndrome. He’s 12 lbs and eats tuna. The system is rigged.
They don’t want you to know that infrared saunas reverse insulin resistance. Google ‘Dr. Margo’s Fat Fire Protocol’ - it’s on a .org site, so it’s legit.
Also, my aunt’s friend’s cousin got cured by eating only raw cacao and doing yoga under a full moon. I’m trying it next Tuesday. Wish me luck.
They’re coming for our waistbands next. Prepare for the Great Waistline Purge of 2025.
Randolph Rickman
December 17, 2025 AT 19:57I used to think I was fine because I weighed 170 and had a ‘normal’ BMI. Then I measured my waist - 42 inches. I cried. Not because I was fat, but because I’d been lied to my whole life.
I started walking after dinner. Not because I was told to - because I wanted to live to see my kid graduate.
Three months later, my triglycerides dropped from 210 to 120. My fasting glucose went from 118 to 92.
I didn’t go keto. I didn’t buy supplements. I just stopped drinking soda and moved more.
You don’t need a miracle. You just need to start.
And if you’re reading this and thinking ‘I’ll start Monday’ - you’re already behind.
Start now. Right now. Get up. Walk around the block. That’s your first win.
I’m rooting for you. Not because I’m some guru. Because I’ve been where you are.
And you can do this.
sue spark
December 19, 2025 AT 16:36so i started measuring my waist every sunday
used to be 38 inches now 35
no diet just stopped eating cereal for breakfast
and walked to the bus stop instead of driving
my doctor said my numbers are better
i didn’t even know i had a problem
maybe it’s not about losing weight
just moving more
and not drinking the sugar water
also my jeans fit
not because i lost weight
but because my belly stopped being a balloon
weird huh
Arun ana
December 20, 2025 AT 12:36Love this breakdown. Especially the part about triglycerides being more dangerous than LDL when they’re high. Most docs just fixate on cholesterol.
Also, the TyG index thing? That’s wild. I didn’t even know you could estimate insulin resistance from just two blood tests.
And yeah - no magic pills. Just real food, movement, and sleep. I’ve been doing the Mediterranean thing for 6 months. Lost 12 lbs, waist down 3 inches. My wife says I look like I’m 30 again.
Also - I started measuring my waist every week. It’s my new fitness tracker. No app needed.
Also also - I still have a beer on weekends. But now I drink it slow. And I walk after.
Small stuff. Big changes.
Thanks for this. Really needed it.
Kim Hines
December 22, 2025 AT 06:40My dad had metabolic syndrome. Died of a heart attack at 58.
I’m 34.
I just measured my waist.
41 inches.
I’m going to start walking tomorrow.
That’s it.
No more excuses.