When your feet feel like they’re on fire, or your hands go numb for no reason, it’s not just aging-it could be peripheral neuropathy. This isn’t a single disease but a group of conditions caused by damage to the nerves outside your brain and spinal cord. These nerves control everything from feeling in your toes to the way your heart beats. When they’re damaged, you don’t just get tingling-you lose balance, struggle to walk, and sometimes can’t sleep because the pain won’t stop.
What Causes Nerve Damage in Peripheral Neuropathy?
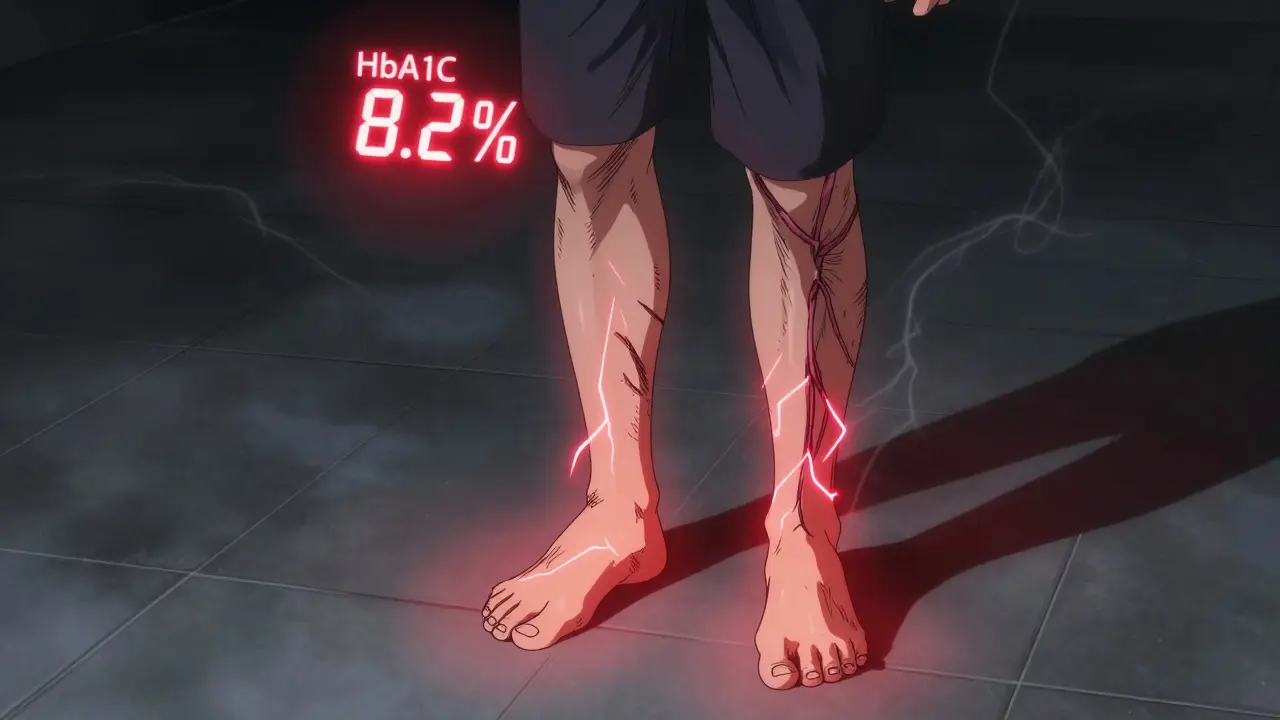
Diabetes is the biggest culprit. About half of all people with diabetes develop some form of nerve damage over time. High blood sugar slowly poisons the nerves, especially in the feet and legs. If your HbA1c stays above 7% for years, your risk climbs sharply. But diabetes isn’t the only cause.
Vitamin B12 deficiency is another common trigger, especially in older adults or people on long-term acid reflux meds. Without enough B12, nerves lose their protective coating. The fix? Simple: monthly injections or high-dose pills can reverse symptoms in 4 to 8 weeks if caught early.
Chemotherapy drugs like vincristine and paclitaxel damage nerves in 30 to 40% of cancer patients. This isn’t just a side effect-it’s often unavoidable, but doctors now monitor nerve function closely during treatment to adjust doses before damage becomes permanent.
Alcohol abuse, autoimmune diseases like Guillain-Barré, infections such as shingles or Lyme disease, and even some inherited disorders can also cause neuropathy. And here’s the tough part: about 20% of cases have no clear cause. These are called idiopathic neuropathies, and they’re the hardest to treat because you can’t fix what you can’t find.
How Do You Know It’s Neuropathy and Not Just Aches?
Neuropathy doesn’t feel like a sore muscle. It’s different. You might describe it as:
- Sharp, stabbing pain like electric shocks
- A constant burning sensation, especially at night
- Tingling or pins-and-needles in your hands or feet
- Feeling like you’re walking on pebbles-even when your shoes are flat
- Loss of balance, tripping often, or dropping things because you can’t feel your fingers
Doctors use simple tests to confirm it. A 10-gram monofilament pressed on your foot checks for loss of sensation. A tuning fork on your big toe tests vibration sense. If you can’t feel either, nerve damage is likely. Nerve conduction studies measure how fast signals travel through your nerves-slower than 40 meters per second means trouble.
Most people don’t get diagnosed until symptoms have been around for 18 months on average. That delay is dangerous. The sooner you start treatment, the better your chances of stopping further damage.
Medications That Actually Work for Neuropathy Pain
Over-the-counter painkillers like ibuprofen or acetaminophen? They barely help. Neuropathic pain doesn’t respond to regular anti-inflammatories. You need drugs that target nerve signals.
Pregabalin (Lyrica) is one of the most prescribed. In clinical trials, 37% of patients got at least 50% pain relief at doses between 150 and 600 mg daily. But it comes with trade-offs: dizziness, weight gain, and brain fog. One patient on Reddit said it cut her pain from 8/10 to 3/10-but she couldn’t drive for two weeks because of dizziness.
Duloxetine (Cymbalta), originally an antidepressant, also works well. About 35% of users report significant pain reduction. But nausea is common-many stop after two weeks because they feel sick.
Amitriptyline, an older tricyclic antidepressant, is cheaper and effective for 41% of users. But side effects are rough: dry mouth in 75%, drowsiness in 60%. It’s often used at night because it helps with sleep too.
None of these are perfect. About 65% of people stop their first neuropathy medication within three months because of side effects. That’s why doctors now recommend starting low and going slow. Don’t expect instant relief-it takes weeks to build up in your system.

Non-Drug Treatments That Make a Real Difference
If pills don’t work-or you can’t tolerate them-there are other options.
Scrambler therapy uses electrical signals to “rewire” how your brain reads pain. After 10 sessions, 85% of patients report at least 50% pain reduction. It’s expensive-$1,200 to $1,500 per full course-but it’s FDA-approved and covered by some insurance.
Spinal cord stimulation implants send mild pulses to your spine to block pain signals. In stubborn cases, 65% of patients get lasting relief. It’s not for everyone, but for those with failed surgeries or uncontrolled pain, it’s life-changing.
Physical therapy isn’t just for injuries. Targeted balance and strength training can cut your fall risk by 30%. Simple exercises like standing on one foot, heel-to-toe walking, and chair stands improve stability. After 12 weeks, most people can walk without holding onto walls.
Custom orthotics and therapeutic shoes are critical for diabetics. Eighty-two percent of users report fewer sores and less pain. The catch? It takes 4 to 6 weeks to get used to them. Most people quit because they feel awkward at first.
Why Controlling Blood Sugar Is the Most Important Step
If you have diabetes and neuropathy, nothing matters more than your HbA1c. The Diabetes Control and Complications Trial showed that keeping it below 7% reduces nerve damage progression by 60%. That’s not a suggestion-it’s the single most effective intervention.
But it’s not just about numbers. You need daily habits: checking your feet twice a day for cuts or blisters, washing them gently, drying thoroughly, and never walking barefoot. Even a tiny blister can turn into a serious infection if you can’t feel it.
New diabetes drugs like SGLT2 inhibitors (e.g., empagliflozin) are now recommended because they not only lower blood sugar but also reduce neuropathy risk by 30%. They’re not magic, but they’re better than older options.
What Doesn’t Work (And Why You Should Avoid It)
Opioids like oxycodone or hydrocodone are sometimes prescribed for severe pain. But studies show they only help 30% of neuropathy patients-and addiction rates jump to over 15% with long-term use. The American Diabetes Association and the American Academy of Neurology both warn against using opioids as a first-line treatment.
Supplements like alpha-lipoic acid or acetyl-L-carnitine are popular online. Some small studies show mild benefit, but they’re not FDA-approved for this use. Don’t waste money unless your doctor recommends them.
And please, don’t ignore symptoms hoping they’ll go away. Neuropathy doesn’t reverse itself. Without treatment, it gets worse. Nerve damage is often permanent.

Living With It: Real Tips from People Who Do
People living with neuropathy share hard-won advice:
- Use a long-handled mirror to check your feet every morning and night.
- Wear socks to bed if your feet burn at night-don’t use heating pads.
- Keep your home clutter-free. Falls are the #1 reason people with neuropathy end up in the ER.
- Use a cane or walker if you’re unsteady. It’s not weakness-it’s safety.
- Join a support group. Reddit’s r/neuropathy has over 12,500 members. Hearing others say “I get it” helps more than you think.
One woman on Healthgrades wrote: “I stopped trying to be ‘normal’ and started focusing on what I could still do. I garden now with gloves and a stool. I can’t run, but I can sit and feel the sun.”
The Future: What’s Coming Next
Research is moving fast. In January 2023, the Foundation for Peripheral Neuropathy launched the Neuropathy Genomics Project to map genetic causes of over 50 types of nerve damage. By 2026, we may be able to test for your specific risk.
Qutenza, a capsaicin patch applied once every 3 months, gives 31% pain relief for many. It’s not a cure, but it’s long-lasting.
Wearable nerve stimulators are in development and could hit the market in 2024. Early trials show 40% pain reduction with daily use.
And AI tools are being trained to spot early signs of nerve damage from simple foot scans or voice patterns-cutting diagnosis time from 18 months to under 6 months.
By 2030, experts predict combination therapies-drugs that both calm nerves and repair them-will become standard. That’s the real hope: not just managing pain, but healing.
Can peripheral neuropathy be cured?
In some cases, yes-if the cause is treatable. For example, correcting a vitamin B12 deficiency or stopping a toxic medication can reverse nerve damage. But if the damage is from long-term diabetes or aging, the goal shifts to stopping further harm and managing symptoms. Nerves heal slowly, if at all, so early action is critical.
Is neuropathy pain constant or does it come and go?
It varies. For many, pain is worse at night and improves during the day. Others have constant burning or tingling. Some experience flare-ups triggered by cold, stress, or standing too long. The pattern often depends on the underlying cause-diabetic neuropathy tends to be steady, while chemotherapy-induced pain can be more unpredictable.
Can I still drive with peripheral neuropathy?
It depends. If you have numbness in your feet, you may not feel the pedals properly. Medications like pregabalin can cause dizziness. Many people adapt by switching to automatic cars, using foot sensors, or avoiding long drives. If you’ve had falls or near-misses, it’s time to talk to your doctor about driving safety.
How long does it take for neuropathy treatments to work?
It varies. Blood sugar control takes 3 to 6 months to show nerve improvement. Vitamin B12 injections can help in 4 to 8 weeks. Medications like pregabalin or duloxetine usually take 2 to 4 weeks to build up in your system. Physical therapy shows results after 8 to 12 weeks. Patience is key-this isn’t a quick fix.
Are there any natural remedies that help?
Some people find relief with acupuncture, massage, or warm baths. Capsaicin cream (from chili peppers) applied to the skin can dull pain for some. But none of these replace medical treatment. Always check with your doctor before trying supplements or alternative therapies-some can interfere with your medications.
What should I do if my pain gets worse suddenly?
Sudden worsening could mean a new problem-like an infection, a pinched nerve, or even a different condition. Don’t wait. Contact your doctor immediately. If you have diabetes and notice redness, swelling, or a sore on your foot, treat it like an emergency. Untreated foot ulcers can lead to amputation.
What Comes Next?
If you’re reading this because you or someone you care about is struggling with numbness, burning, or balance issues-don’t wait. See a neurologist or a specialist in peripheral neuropathy. Bring a list of your symptoms, your medications, and your blood sugar logs if you’re diabetic.
Start with the basics: check your feet daily, get your HbA1c tested, and ask about nerve conduction studies. You don’t have to live with pain that keeps you awake at night. The right treatment exists-you just need to find it.
And remember: this isn’t just about pain. It’s about staying independent. Walking without fear. Sleeping through the night. Keeping your job. Those are the real goals-and they’re possible, even with nerve damage.

Coy Huffman
February 4, 2026 AT 12:06Kunal Kaushik
February 5, 2026 AT 04:05Harriot Rockey
February 5, 2026 AT 16:58Caleb Sutton
February 6, 2026 AT 23:07Jamillah Rodriguez
February 8, 2026 AT 08:00Susheel Sharma
February 9, 2026 AT 02:53Rachel Kipps
February 10, 2026 AT 00:26Wendy Lamb
February 11, 2026 AT 03:57Katherine Urbahn
February 11, 2026 AT 17:56Justin Fauth
February 13, 2026 AT 10:41Joy Johnston
February 13, 2026 AT 22:14