When your lungs start to feel heavy, your cough won’t quit, and breathing feels like a chore, it’s not just a bad cold. It could be pneumonia - and not all types are the same. Knowing whether it’s bacterial, viral, or fungal isn’t just medical jargon. It changes everything: how you’re treated, how long you’ll be sick, and even whether antibiotics will help or hurt.
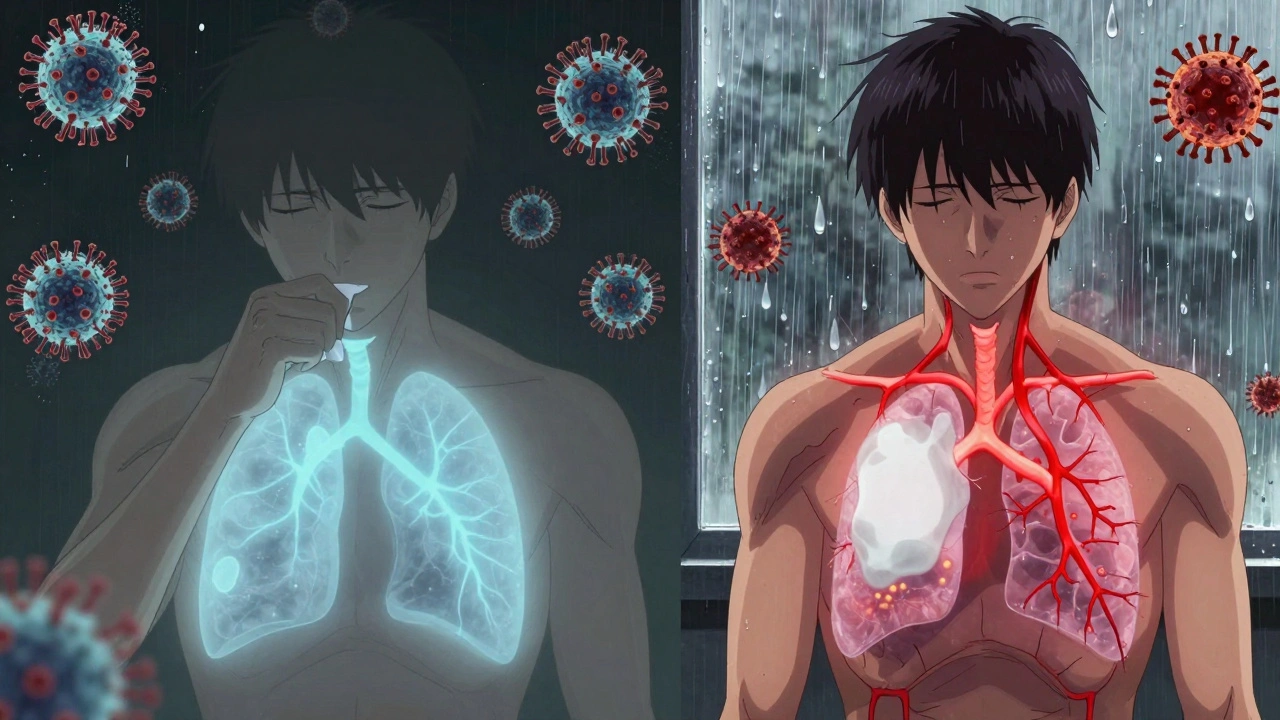
What Pneumonia Actually Does to Your Lungs
Pneumonia isn’t just a cough with a fever. It’s an infection that fills the tiny air sacs in your lungs - called alveoli - with fluid or pus. That’s why breathing becomes hard. Your body’s trying to fight off invaders, but the inflammation and gunk clog up the space where oxygen should be entering your blood. The result? You feel tired, short of breath, and sometimes blue around the lips because your body isn’t getting enough oxygen.
The big difference between types of pneumonia? The germ causing it. Bacteria, viruses, and fungi each behave differently. They attack in different ways, show up differently on scans, and need totally different treatments. Getting the wrong treatment doesn’t just waste time - it can make things worse.
Bacterial Pneumonia: The Sudden, Severe Type
Bacterial pneumonia hits fast. One day you might feel fine; the next, you’re running a high fever - 102°F to 105°F - with chills, chest pain, and a cough that brings up thick, yellow, green, or even bloody mucus. Your heart races. Your fingers or lips turn bluish. This isn’t just a bad flu. This is your body in full alarm mode.
The most common culprit? Streptococcus pneumoniae. It’s responsible for about half of all community-acquired pneumonia cases worldwide. Other bacteria like Staphylococcus aureus, Haemophilus influenzae, and Legionella pneumophila (which causes Legionnaires’ disease) also show up, especially in older adults or people with weak immune systems.
On a chest X-ray, bacterial pneumonia usually looks like a solid white patch - called lobar consolidation - in one part of the lung. That’s because the infection is localized, not spread out. Doctors can often tell it’s bacterial just by how quickly symptoms come on and what the X-ray shows.
Treatment? Antibiotics. Penicillin, macrolides like azithromycin, or fluoroquinolones like levofloxacin are common choices. If it’s caught early, most people start feeling better in 48 to 72 hours. But if it’s severe, hospitalization is needed. About 5 to 7% of hospitalized patients with bacterial pneumonia don’t survive - especially if they’re over 65 or have other health problems like diabetes or COPD.
Viral Pneumonia: The Slow Burn
Viral pneumonia doesn’t hit like a sledgehammer. It creeps in. You might start with a runny nose, sore throat, or mild headache - classic cold symptoms. Then, over 3 to 5 days, it moves deeper. You develop a dry cough that gets worse. Your fever stays low to moderate - usually between 100°F and 102°F. Muscle aches, fatigue, and a general feeling of being wrecked are common.
The usual suspects? Influenza (flu), respiratory syncytial virus (RSV), and SARS-CoV-2 (the virus behind COVID-19). Rhinovirus and human metapneumovirus are also frequent causes, especially in kids and older adults.
On an X-ray, viral pneumonia looks different. Instead of one solid white patch, you see a hazy, scattered pattern across both lungs. That’s because viruses spread more evenly through the lung tissue, triggering inflammation in the walls of the air sacs rather than filling them with pus.
Antibiotics? Useless. They don’t kill viruses. For flu, antivirals like oseltamivir (Tamiflu) can help if taken within 48 hours of symptoms. For severe COVID-19 pneumonia, remdesivir may be used in hospitals. But most of the time, treatment is supportive: rest, fluids, fever reducers, and oxygen if needed.
Here’s the scary part: viral pneumonia can open the door to bacterial pneumonia. About 25 to 30% of people with severe flu develop a secondary bacterial infection - often from Streptococcus pneumoniae or Staphylococcus aureus. That’s why doctors watch closely after a viral illness. If your fever comes back after seeming to improve, or your cough turns wet and thick, it might be a bacterial takeover.
Fungal Pneumonia: The Hidden Threat
Fungal pneumonia is rare in healthy people. But if you’re immunocompromised - due to HIV, cancer treatment, organ transplants, or long-term steroid use - it becomes a real danger. Even if you’re not sick, you might have breathed in spores without knowing it. Fungi like Coccidioides (Valley fever), Histoplasma capsulatum, and Blastomyces dermatitidis live in soil, bird droppings, and bat guano.
People who work outdoors - farmers, landscapers, construction workers - are at higher risk. In areas like the southwestern U.S., where Valley fever is common, up to 20,000 cases are reported every year. In South Africa, where dust storms and soil disturbance are frequent, cases are rising too.
Symptoms? Fever, cough with phlegm, chest pain, night sweats, and sometimes nausea or diarrhea. It can mimic bacterial or viral pneumonia, which is why it’s often missed. Diagnosis requires special tests - sputum cultures, blood tests, or even lung biopsies - because regular chest X-rays can look normal early on.
Treatment isn’t antibiotics. It’s antifungals: amphotericin B for severe cases, or azoles like fluconazole or itraconazole for long-term control. Recovery takes weeks to months. And in people with weakened immune systems, fungal pneumonia can be deadly - with mortality rates between 10% and 15%.
How Doctors Tell Them Apart
Doctors don’t guess. They use clues:
- Speed of onset: Bacterial = sudden. Viral = gradual. Fungal = slow and persistent.
- Fever: Bacterial = high (102°F+). Viral = low to moderate. Fungal = variable, often low-grade.
- Cough: Bacterial = wet, colored mucus. Viral = dry, worsening over days. Fungal = may be dry or produce thick mucus.
- X-ray pattern: Bacterial = one solid white area. Viral = hazy, spread out. Fungal = patchy or nodular, sometimes with cavities.
- Lab tests: Blood tests, sputum cultures, PCR panels, and antigen tests now let doctors identify the pathogen within hours.
Modern multiplex PCR tests can check for 20+ viruses and bacteria from one nasal swab. That’s a game-changer. No more guessing. No more unnecessary antibiotics.

Prevention: What Actually Works
Not all pneumonia is preventable - but a lot is.
- For bacterial pneumonia: The pneumococcal vaccine (PCV15, PCV20, PPSV23) cuts risk by 60-70% in kids and 45-75% in adults over 65. Yet only 68% of seniors get it. That’s too low.
- For viral pneumonia: The flu shot reduces pneumonia risk by 40-60% in good match years. The COVID-19 vaccine cuts pneumonia risk by up to 90% in the first few months after vaccination.
- For fungal pneumonia: Avoid digging in soil or disturbing bird/bat droppings if you’re immunocompromised. Wear an N95 mask in dusty environments. No vaccine exists yet.
Smoking increases your risk of pneumonia by 2.3 times. Quitting - even late in life - lowers your risk fast. If you have asthma, COPD, or diabetes, managing those conditions is just as important as vaccines.
Why Getting It Right Matters
Every year in the U.S., pneumonia leads to 1 million hospital stays and 50,000 deaths. Around 30% of outpatient antibiotic prescriptions are unnecessary - mostly because viral pneumonia is mistaken for bacterial. That’s not just wasteful. It fuels antibiotic resistance. The CDC says inappropriate antibiotic use increases resistant infections by 35% in communities.
When you take an antibiotic for a virus, you’re not helping yourself. You’re helping superbugs survive. Those bugs then spread to others - even people who never took antibiotics.
Accurate diagnosis saves lives. It saves money. It protects the next generation from untreatable infections.
What to Do If You Suspect Pneumonia
If you have:
- Fever over 101°F with chills
- Cough that lasts more than 7 days or gets worse
- Shortness of breath at rest
- Chest pain when breathing or coughing
- Bluish lips or fingertips
See a doctor. Don’t wait. Don’t assume it’s just a cold. Get a chest X-ray and ask about testing. Tell your doctor if you’ve been around sick people, traveled recently, work outdoors, or have a weak immune system.
Early action makes all the difference. Whether it’s antibiotics, antivirals, or antifungals - the right treatment starts with knowing what you’re fighting.
Can you have pneumonia without a fever?
Yes, especially in older adults, young children, or people with weakened immune systems. In these groups, pneumonia may show up as confusion, dizziness, low energy, or a drop in body temperature instead of a fever. Don’t wait for a high fever to seek help.
Is viral pneumonia contagious?
Yes. Viral pneumonia spreads the same way as colds and flu - through coughs, sneezes, and touching contaminated surfaces. You can spread the virus even before you feel sick. That’s why handwashing, masks, and staying home when ill are critical.
How long does pneumonia last?
Bacterial pneumonia improves in 1-3 weeks with antibiotics. Viral pneumonia can take 2-6 weeks to fully clear, even after the fever breaks. Fungal pneumonia often needs months of treatment and can linger for a year or more in immunocompromised people. Fatigue and cough can hang on long after the infection is gone.
Can pneumonia come back after treatment?
Yes. If you didn’t finish your antibiotics, the infection can return stronger. People with chronic lung disease, smoking habits, or weakened immunity are at higher risk for recurrence. Follow-up X-rays are often needed to make sure the lungs have fully cleared.
Do I need a chest X-ray for pneumonia?
Not always - but if symptoms are severe, last more than a week, or you’re over 65 or have other health issues, an X-ray is essential. It confirms pneumonia, shows how bad it is, and helps tell bacterial from viral. Without it, you’re guessing.


Libby Rees
December 4, 2025 AT 11:27Great breakdown. I work in public health and see too many people assume antibiotics fix everything. This post should be mandatory reading.
Carolyn Ford
December 5, 2025 AT 09:23Actually, the CDC data on antibiotic misuse is outdated-2023 reports show it’s closer to 40%, not 30%. And you ignored fungal pneumonia in immunocompetent travelers to endemic zones. This is sloppy.
Rudy Van den Boogaert
December 6, 2025 AT 19:59My dad had fungal pneumonia after a dust storm in Arizona. Took six months to recover. No one believed him until his sputum culture came back. It’s not rare if you’re around dirt or birds. Just underdiagnosed.
Alex Piddington
December 7, 2025 AT 23:52Thanks for sharing this. As a nurse, I’ve seen too many elderly patients dismissed because they didn’t have a fever. This is exactly the kind of clarity we need in patient education. 💙
Dematteo Lasonya
December 9, 2025 AT 18:59I’m so glad you mentioned the long tail of fatigue after viral pneumonia. I was told I was ‘just tired’ for months after COVID. Turns out my lungs were still healing. This helped me understand why.
Jordan Wall
December 10, 2025 AT 13:53IMO, the real issue here is the lack of point-of-care multiplex PCR deployment in primary care. We're still operating in the 2010s while the tech exists. Also, PCV20 is underutilized due to payer barriers-not patient ignorance. #HealthSystemsFail
michael booth
December 12, 2025 AT 11:03Heidi’s right about the CDC stat-but your point about fungal pneumonia in outdoor workers is spot on. I’m a landscaper and we all joke about ‘Arizona lung’ but no one talks about it. Maybe we need a workplace awareness campaign?
Heidi Thomas
December 14, 2025 AT 01:37Stop pretending viral pneumonia is harmless. It’s the silent killer that leads to bacterial superinfections. And if you think vaccines are 90% effective, you haven’t looked at the real-world data from last winter. Most people who got pneumonia were vaccinated. The numbers lie.
Gillian Watson
December 15, 2025 AT 00:41My mum had pneumonia at 78 and didn’t have a fever. Just kept falling asleep in her chair. Took three visits to the doctor before they did the X-ray. This post saved me from dismissing her symptoms again.