Restless Legs Syndrome (RLS) isn't just about discomfort-it's a neurological condition that steals sleep, disrupts daily life, and leaves many feeling trapped in their own bodies. If you've ever felt an irresistible urge to move your legs while lying down, accompanied by crawling, tingling, or aching sensations, you're not alone. About 1 in 10 adults in North America and Europe live with this condition, and for many, the first treatment they're offered is a dopaminergic medication. But here’s the truth most doctors don’t tell you upfront: dopaminergic medications may help in the short term, but they can make your RLS worse over time.
What Exactly Is Augmentation?
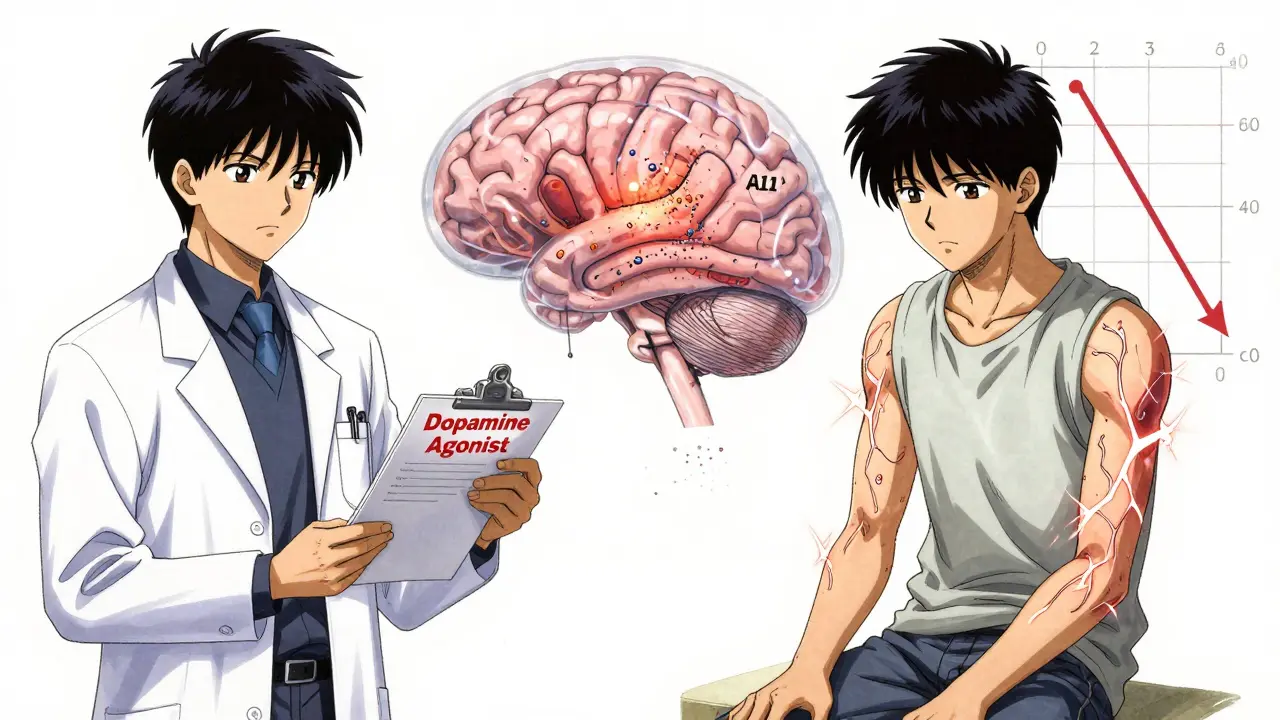
When doctors first started prescribing dopamine agonists like pramipexole (Mirapex) and ropinirole (Requip) for RLS, they worked wonders. Symptoms vanished. Patients slept. Life improved. But within a year or two, something strange started happening. Symptoms didn’t just come back-they got worse. They started earlier in the day. They spread from the legs to the arms. The urge to move became constant, not just at night. This isn’t a coincidence. It’s called augmentation.Augmentation is when RLS symptoms change in a predictable, harmful way because of long-term dopamine agonist use. Studies show that 40% to 60% of patients on these drugs develop augmentation within 1 to 3 years. By the fifth year, that number climbs to nearly 80%. It’s not rare. It’s expected. And it’s not just a side effect-it’s a direct consequence of how these drugs interact with the brain’s dopamine system. The very mechanism that relieves symptoms at first ends up dysregulating it.
Think of it like this: Your brain has a delicate balance of dopamine in a region called the A11, which controls leg movement. Dopamine agonists flood this area, tricking the brain into thinking it has enough. Over time, the brain adapts by reducing its own dopamine production and sensitivity. When that happens, symptoms rebound harder, earlier, and in new places. That’s augmentation. And once it starts, it’s extremely hard to reverse.
Why Dopamine Agonists Are No Longer First-Line
In 2024, the American Academy of Sleep Medicine updated its guidelines-and it was a game-changer. They no longer recommend dopamine agonists as the first treatment for RLS. Why? Because the evidence became undeniable. A 2023 meta-analysis in JAMA Neurology compared pramipexole and pregabalin over a full year. At 12 weeks, both worked similarly. But at 52 weeks? Pregabalin still worked. Pramipexole? Its effectiveness dropped by 35% because of augmentation.Doctors who still prescribe these drugs as a first choice are following outdated protocols. The FDA added black box warnings to all dopamine agonists in 2022, specifically calling out augmentation risk. The European Medicines Agency followed with similar restrictions. Even the Restless Legs Syndrome Foundation now states clearly on its website: “Dopaminergic medications are now second-line therapy due to augmentation.”
And it’s not just about worsening symptoms. These drugs carry real risks of impulse control disorders. One study found 6.1% of RLS patients on dopamine agonists developed compulsive gambling, shopping, or binge eating-rates 12 times higher than the general population. That’s not a minor side effect. That’s life-altering.
What Works Better Now?
The new standard for first-line treatment is alpha-2-delta ligands. These include gabapentin enacarbil (Horizant) and pregabalin (Lyrica). They don’t touch dopamine. Instead, they calm overactive nerve signals in the spinal cord. And crucially, they don’t cause augmentation.Gabapentin enacarbil, approved by the FDA in 2011, reduces RLS symptoms by 40-60% on the International Restless Legs Syndrome Study Group (IRLSSG) scale. Pregabalin works just as well in head-to-head trials. The catch? They take time. You won’t feel relief the first night. It takes 5 to 14 days for full effect. But once they kick in, they hold steady. No worsening. No spread to arms. No rebound.
Compare this to dopamine agonists: they work fast-within 30 to 60 minutes. That’s why they were so popular. But speed comes at a cost. For someone with RLS only 2 or 3 nights a week, a low-dose dopamine agonist might still make sense. But for daily symptoms? It’s a trap.
Other Options You Should Know
Not everyone responds to alpha-2-delta ligands. Some people get dizzy or gain weight. Others need something stronger. Here are two alternatives with solid evidence:- Low-dose opioids: Oxycodone at 5 mg daily can reduce symptoms by 50-70%. Yes, opioids. But here’s the twist: when used at very low doses specifically for RLS, addiction risk is extremely low-just 0.8% in one study. This is not about pain management. It’s about controlling neurological symptoms. Still, it’s not for everyone. Avoid if you have a history of substance use.
- Carbidopa-levodopa (Sinemet): This combo works well for occasional RLS, like before a long flight. But if you take it daily for more than 6 months, 70% of patients develop augmentation. So it’s strictly for “as-needed” use.
And then there’s iron. RLS is strongly linked to low iron in the brain-even if your blood iron looks normal. If your serum ferritin is below 75 mcg/L, oral iron supplements (100-200 mg elemental iron daily) can cut symptoms by 35% in 12 weeks. It’s simple, cheap, and safe. Yet most patients never get tested.
Non-Medication Strategies That Actually Help
Medication isn’t the whole story. Many people don’t realize how much lifestyle changes can reduce symptoms. Here’s what the data says:- Caffeine: 80% of RLS patients consume caffeine daily. Cutting it out can reduce symptoms by 20-30%.
- Alcohol: It worsens symptoms in 65% of users. Even one drink at night can trigger or amplify RLS.
- Sleep hygiene: Consistent sleep schedule, cool room temperature, and avoiding screens before bed improve sleep quality and reduce RLS episodes.
- Exercise: Moderate activity like walking or cycling during the day helps. But intense workouts right before bed? That can make things worse.
One patient on the RLS Foundation forum wrote: “I stopped drinking coffee after 8 PM, started taking iron, and got off Mirapex. My symptoms dropped by 70% in three weeks. I didn’t need anything else.”

What to Do If You’re Already on Dopamine Agonists
If you’ve been on pramipexole or ropinirole for more than 6 months and your symptoms are getting worse-earlier in the day, spreading to your arms, feeling more intense-you’re likely experiencing augmentation. Don’t panic. But don’t keep increasing the dose. That’s the worst thing you can do.Work with your doctor on a taper plan. Reduce the dose by 25% every 1-2 weeks. At the same time, start an alpha-2-delta ligand like gabapentin enacarbil. Studies show that 85% of patients successfully switch without major rebound when done this way. Abruptly stopping dopamine agonists can cause severe withdrawal symptoms, so never do it alone.
Also, get your ferritin level checked. If it’s under 75, start iron supplements. Many patients don’t realize their RLS is tied to low iron-not just brain chemistry.
The Future of RLS Treatment
The treatment landscape is shifting fast. In 2024, dopamine agonists made up only 20% of new RLS prescriptions, down from 75% in 2010. Alpha-2-delta ligands now lead the market, with 65% of new prescriptions. Experts agree: long-term dopamine therapy is outdated.Research is moving toward solutions that target the root cause-brain iron deficiency. Three new clinical trials are underway, testing drugs that deliver iron directly to the brain, and a new selective dopamine agonist designed to avoid augmentation. Non-drug options like transcranial magnetic stimulation are also being studied.
But here’s the bottom line: if you have daily RLS, don’t wait for augmentation to hit. Talk to your doctor about switching to a safer, more sustainable option. You don’t have to live with sleepless nights. And you don’t have to risk making your condition worse with a drug that was once considered a miracle-but now, for most people, is a trap.
Are dopamine agonists still used for Restless Legs Syndrome?
Yes, but only in limited cases. Dopamine agonists like pramipexole and ropinirole are no longer first-line treatments due to high risk of augmentation and impulse control disorders. They’re now reserved for patients with infrequent symptoms (less than 3 nights per week) or those who can’t tolerate other medications. Even then, treatment is limited to 6 months or less.
What is augmentation in Restless Legs Syndrome?
Augmentation is a worsening of RLS symptoms caused by long-term use of dopamine agonists. Symptoms begin earlier in the day (often 2-6 hours sooner), spread from the legs to the arms, become more intense, and occur more frequently-sometimes daily. It affects 40-60% of patients within 1-3 years of treatment and up to 80% after five years.
What are the best medications for RLS today?
Alpha-2-delta ligands like gabapentin enacarbil (Horizant) and pregabalin (Lyrica) are now first-line treatments. They reduce symptoms by 40-60% without causing augmentation. Low-dose opioids (e.g., oxycodone 5 mg) are effective for severe cases with low addiction risk. Iron supplements are recommended if serum ferritin is below 75 mcg/L.
Can RLS be managed without medication?
Yes, for many people. Reducing caffeine, avoiding alcohol, improving sleep hygiene, and taking iron supplements (if deficient) can reduce symptoms by 20-35%. Regular moderate exercise during the day also helps. These changes are often the first step before medication is even considered.
How do I know if my RLS is getting worse because of my medication?
If your symptoms started earlier in the day (e.g., now at 3 PM instead of 8 PM), spread to your arms or torso, feel more intense, or occur more than 5 nights a week, you may be experiencing augmentation. This usually happens after 6-12 months of dopamine agonist use. Talk to your doctor immediately-don’t increase your dose.


Marie Fontaine
February 10, 2026 AT 07:51OMG this is so real 😭 I was on Mirapex for 2 years and thought I was getting worse because I was ‘aging’-turns out it was the drug. Switched to pregabalin and iron supplements, and my legs finally chill at night. No more 2 AM sprinting around the living room. Also, cut out coffee after 6 PM and it’s like a whole new life. 💪
Ryan Vargas
February 12, 2026 AT 00:07It’s not merely a medical issue-it’s a systemic betrayal. The pharmaceutical-industrial complex has spent decades promoting dopamine agonists as panaceas while burying the long-term data. The FDA’s black box warning? A reactive gesture, not a preventive one. We’re witnessing a calculated erosion of neurochemical homeostasis under the guise of treatment. The brain doesn’t ‘adapt’-it’s hijacked. Dopamine isn’t just a neurotransmitter; it’s the conductor of the symphony of movement, and these drugs don’t tune the instrument-they smash it. The 80% augmentation rate after five years isn’t a side effect-it’s the intended outcome for repeat prescriptions. Who profits? Not you. Not me. Always the shareholders.
Tori Thenazi
February 12, 2026 AT 23:14Wait… so you’re telling me… the doctors… knew? And they STILL prescribed it? 🤯 I’m not even mad… I’m just… shocked. My neurologist said ‘it’s the gold standard’-but now I’m reading that the gold standard is actually a trapdoor? And the FDA warning? They didn’t even mention it. I feel so violated. Also-did you know they used to give RLS patients Adderall? Like, for real. I’m not kidding. I found an old forum post from 2008. Someone said their doctor said ‘it’ll help you focus too.’ I’m crying. I’m laughing. I’m filing a complaint.
Ashlyn Ellison
February 14, 2026 AT 14:41I’ve had RLS since 2015. Tried everything. Dopamine meds made it worse. Iron supplements (150mg elemental) fixed 70% of it. No joke. My ferritin was 42. Now it’s 98. Sleep is back. I didn’t need a prescription. Just a blood test. Why isn’t this the first thing every doctor checks?
THANGAVEL PARASAKTHI
February 16, 2026 AT 04:53hey man this is so useful, i never knew iron was linked to rls. i thought it was just nerves or stress. i got my ferritin checked last week-48. gonna start iron today. thanks for the heads up. also, i cut out soda and my legs are way calmer. small changes, big difference 😊
Chelsea Deflyss
February 17, 2026 AT 05:30Ugh. I hate when people act like this is new info. I’ve been saying this for years. My cousin’s neurologist told her the same thing in 2019. She went off pramipexole, started gabapentin, and now she’s biking every morning. Meanwhile, my sister is still on it, and now she’s got compulsive shopping debt and can’t sleep past 3am. Wake up, people.
Tricia O'Sullivan
February 18, 2026 AT 22:55Thank you for presenting this information with such clarity and rigor. The shift in clinical guidelines is not merely a trend-it is a necessary recalibration grounded in longitudinal evidence. I have observed in my practice that patients who transition from dopamine agonists to alpha-2-delta ligands report not only symptom improvement, but a restoration of autonomy. The emotional relief is as profound as the physiological. I commend your thoroughness.
Scott Conner
February 20, 2026 AT 02:56so wait-so if i take sinemet for a flight, i’m okay? like, just once in a while? or is that still risky? i’m scared to even ask my doc. they act like i’m asking for heroin.
Alex Ogle
February 20, 2026 AT 16:00I used to think I was just ‘weird’ for needing to walk around at 1am. Then I found out my legs were screaming for iron. I started taking 130mg of elemental iron nightly. Three weeks later, I slept 8 hours straight for the first time in a decade. No meds. No drama. Just… peace. If you’re reading this and you have RLS-get your ferritin tested. It’s a $15 blood test. Don’t let them push pills on you before they check the basics. Your future self will thank you.
Brandon Osborne
February 21, 2026 AT 12:50THIS IS WHY I HATE MODERN MEDICINE. THEY DON’T CARE ABOUT YOU. THEY CARE ABOUT THE NEXT PRESCRIPTION. I WAS ON MIRAPEX FOR 4 YEARS. MY ARMS STARTED MOVING. I HAD TO QUIT MY JOB BECAUSE I COULDN’T SIT STILL. MY DOCTOR SAID ‘JUST INCREASE THE DOSE.’ I DID. IT GOT WORSE. THEN I FOUND THIS POST. NOW I’M ON GABAPENTIN AND IRON. I’M NOT JUST BETTER-I’M ALIVE AGAIN. IF YOU’RE ON DOPAMINE DRUGS AND YOUR SYMPTOMS ARE GETTING WORSE-YOU’RE NOT CRAZY. YOU’RE BEING POISONED. STOP TAKING IT. TALK TO YOUR DOCTOR. OR FIND A NEW ONE.
Lyle Whyatt
February 22, 2026 AT 05:29As someone who’s been managing RLS since my 20s, I’ve tried the whole spectrum-from dopamine agonists to acupuncture to weighted blankets. The only thing that stuck? Iron. My ferritin was 38. Now it’s 102. I don’t even take meds anymore. I walk every morning, avoid caffeine after noon, and sleep like a baby. The real tragedy? Most docs don’t even check ferritin. It’s like diagnosing diabetes and ignoring blood sugar. I’m not mad-I’m just… disappointed. We deserve better.