When a drug leaves the lab and enters the market, it must remain safe and effective for months or even years. That’s not magic-it’s stability testing. This isn’t optional. It’s a legal requirement. If a pill degrades in heat or a liquid freezes during shipping, patients could get less medicine-or worse, harmful byproducts. Stability testing answers one simple question: Will this drug still work when it reaches the patient?
Why Temperature and Time Matter
Pharmaceuticals don’t sit still. Heat, humidity, and time cause chemical changes. A tablet might lose potency. A liquid might separate. A biologic might clump together. These changes don’t always show up in the lab right away. That’s why stability testing runs for months-or years-under controlled conditions that mimic real-world storage. The global standard is ICH Q1A(R2), set by the International Council for Harmonisation in 2003. It’s followed by the FDA, EMA, Health Canada, and most major regulators. The goal? Make sure a drug works the same way whether it’s sold in Cape Town, Tokyo, or Toronto.Long-Term Testing: The Real-World Clock
Long-term testing is the backbone of stability. It’s what determines the expiration date. Two main conditions are used:- 25°C ± 2°C and 60% RH ± 5% RH - This mimics temperate climates like the U.S. or Europe.
- 30°C ± 2°C and 65% RH ± 5% RH - This matches hot, humid regions like Southeast Asia or Africa.
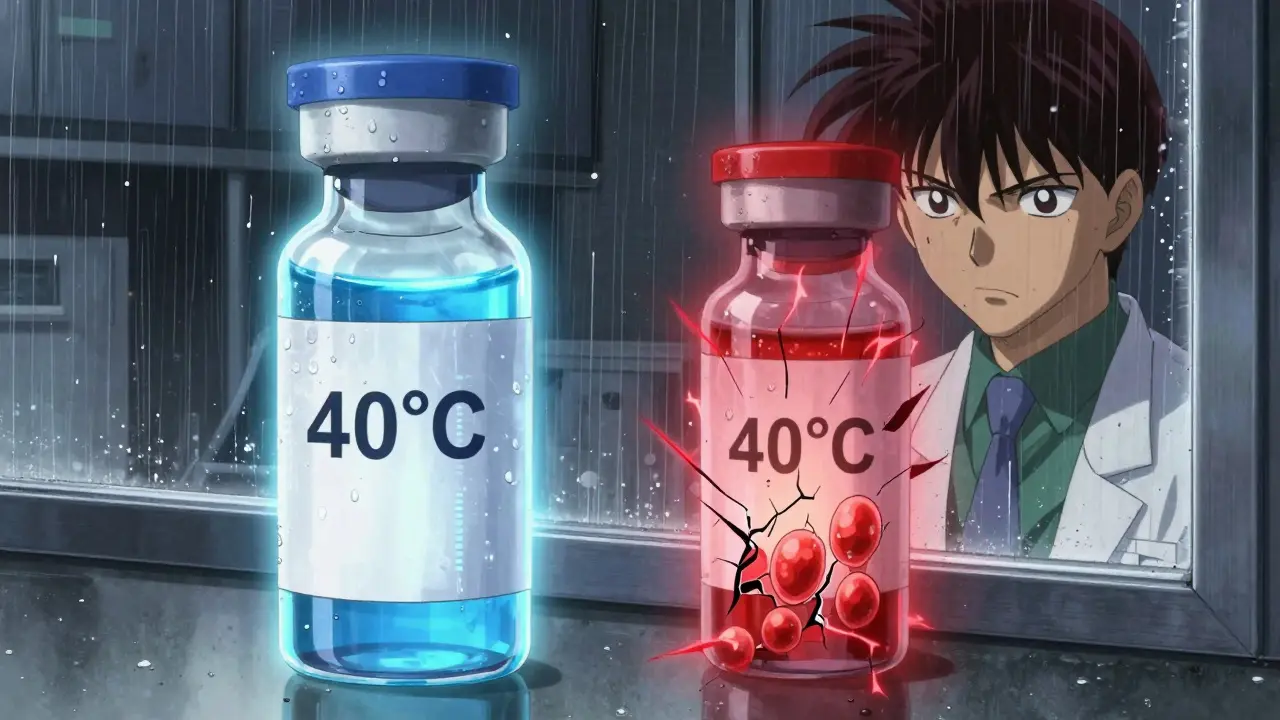
Accelerated Testing: The Speed Test
Accelerated testing is like putting a drug through a stress test. It’s not meant to predict real-life aging-it’s meant to find problems fast. The condition? 40°C ± 2°C and 75% RH ± 5% RH for six months. That’s hotter and wetter than any warehouse or pharmacy. If the drug fails here, you know there’s a serious risk. This test is required for all solid oral products. If the drug passes, you can use the data to estimate shelf life. If it fails, you must run more tests or change the formula.Intermediate Testing: The Safety Net
Intermediate testing is only needed if two things happen:- You’re using 25°C/60% RH for long-term testing (not 30°C).
- Accelerated testing shows a significant change.
Refrigerated and Frozen Products
Not all drugs are kept at room temperature. Insulin, vaccines, and many biologics need cold storage. For refrigerated products:- Long-term: 5°C ± 3°C for 12 months.
- Accelerated: 25°C ± 2°C and 60% RH ± 5% RH for 6 months.
Global Zones and Regional Differences
The world isn’t one climate. ICH defines five climatic zones:- Zone I: Temperate - 21°C / 45% RH
- Zone II: Mediterranean/Subtropical - 25°C / 60% RH
- Zone III: Hot-Dry - 30°C / 35% RH
- Zone IVa: Hot-Humid/Tropical - 30°C / 65% RH
- Zone IVb: Hot/Higher Humidity - 30°C / 75% RH
What Counts as a “Significant Change”?
This is where things get messy. ICH Q1A(R2) says a product has failed if:- Assay changes by more than 5%
- Any impurity exceeds its specification limit
- Physical properties change noticeably (color, texture, dissolution rate)
Equipment and Environment Control
Stability chambers aren’t fancy fridges. They’re precision instruments. They must hold temperature within ±0.5°C and humidity within ±2% RH. If they drift, the data is invalid. Chambers need qualification: IQ (Installation Qualification), OQ (Operational Qualification), and PQ (Performance Qualification). That’s a 3-week process per chamber. Temperature mapping is critical. In a large chamber, shelves on the top might be 1.8°C warmer than the bottom. If you only test one shelf, you’re not testing the whole batch.Real-World Failures and Consequences
Stability failures aren’t theoretical. In 2021, Teva recalled 150,000 vials of Copaxone® because their stability test missed aggregation at 40°C. The drug clumped, reducing effectiveness. In 2022, the FDA issued 27 warning letters for stability testing violations. Most cited inadequate protocols, poor documentation, or unvalidated equipment. One biotech lost $4 million when their mRNA vaccine’s lipid nanoparticles degraded during transport. The standard 40°C test didn’t catch it-because the real problem was freeze-thaw cycles, not heat.
What’s Changing? The Future of Stability Testing
The ICH Q1A(R2) standard is 20 years old. It was made for pills and syrups. Today’s drugs are complex: monoclonal antibodies, gene therapies, mRNA vaccines. New tools are emerging:- Predictive modeling: Using AI to simulate degradation at 50-80°C. Some companies cut testing time by 9-12 months.
- Real-time release testing: Using sensors during manufacturing to predict shelf life without waiting months.
- Dynamic humidity testing: Instead of constant 65% RH, test how products react to daily humidity swings-something that happens in warehouses.
What You Need to Do
If you’re developing a drug:- Decide your target markets. Pick your long-term condition (25°C or 30°C).
- Run accelerated testing at 40°C/75% RH for 6 months.
- If you’re using 25°C for long-term, run intermediate testing at 30°C/65% RH if accelerated fails.
- Test at 0, 3, 6, 9, 12, 18, 24, and 36 months.
- Use calibrated chambers with ±0.5°C and ±2% RH control.
- Document everything. Every temperature log, every result, every deviation.
Common Mistakes to Avoid
- Testing only at room temperature when selling in tropical regions.
- Ignoring humidity. Most failures are from moisture, not heat.
- Using unqualified chambers. If the temp drifts, your whole study is invalid.
- Waiting until the last minute to start testing. Stability studies take years.
- Assuming accelerated results = real-time results. They don’t always match, especially for biologics.
Final Thought
Stability testing isn’t about checking boxes. It’s about protecting people. A pill that looks fine might be 10% weaker. A vaccine that’s been in a hot truck might not work at all. The temperature and time conditions aren’t arbitrary-they’re the line between a safe medicine and a dangerous one. The rules haven’t changed in 20 years. But the drugs have. The challenge now isn’t just following the rules-it’s knowing when they’re no longer enough.What are the standard temperature and humidity conditions for long-term stability testing?
The two standard conditions are 25°C ± 2°C with 60% RH ± 5% RH, or 30°C ± 2°C with 65% RH ± 5% RH. The choice depends on the target market’s climate zone. For tropical regions, 30°C/65% RH is required. Both are defined under ICH Q1A(R2) and used globally by regulators like the FDA and EMA.
How long does stability testing typically take?
Long-term stability testing runs for at least 12 months at submission, but full shelf-life studies often continue to 24 or 36 months. Accelerated testing lasts 6 months at 40°C/75% RH. Intermediate testing, if needed, also runs for 6 months. Because data is collected over time, companies often start testing years before launch.
Why is accelerated testing done at 40°C and 75% RH?
The 40°C/75% RH condition was chosen because it’s extreme enough to accelerate degradation without melting excipients or causing unrealistic chemical reactions. It simulates worst-case shipping or storage scenarios. Studies show this condition correlates to about 24 months of real-time storage at 25°C/60% RH for most small-molecule drugs, though it’s less reliable for hygroscopic or biologic products.
Do refrigerated drugs follow the same stability rules?
No. Refrigerated products are tested at 5°C ± 3°C for long-term storage. Their accelerated condition is 25°C ± 2°C and 60% RH ± 5% RH-not 40°C. This reflects real-world risks like power outages or transport delays, not extreme heat. Freeze-thaw cycles are also tested for frozen products like mRNA vaccines.
What happens if a stability test fails?
A failed stability test can lead to regulatory actions: warning letters, product recalls, or denial of approval. For example, in 2021, Teva recalled 150,000 vials of Copaxone® after stability testing revealed aggregation at 40°C. Companies must investigate the cause, update their formulation or storage conditions, and often restart testing-delaying launch by months or years.
Are there new trends changing stability testing?
Yes. Predictive modeling using AI and high-temperature stress tests (50-80°C) is reducing testing time by 9-12 months for some products. Real-time release testing and dynamic humidity testing are also emerging. However, regulators like the EMA still require physical data for approval. The ICH is working on updates to Q1A(R2) to address complex products like antibody-drug conjugates and cell therapies.


Jenny Salmingo
January 1, 2026 AT 20:39Just think about how many people rely on these pills to feel normal. It’s wild that we take it for granted that the medicine won’t fall apart in a hot car. Thanks for laying this out so clearly.
Frank SSS
January 2, 2026 AT 15:26Okay but let’s be real - most of these stability tests are just corporate box-ticking. I’ve seen labs skip humidity controls because ‘it’s too expensive.’ And yeah, the FDA catches some, but not all. The system’s broken, and we’re all just pretending it’s not.
Paul Huppert
January 4, 2026 AT 13:47Interesting point about the 4.8% potency drop triggering a hold. That’s so subtle but so telling. It’s not just the number - it’s the trend. Makes you wonder how many drugs slip through because the data looks ‘fine’ on paper.
Emma Hooper
January 6, 2026 AT 12:29Ugh, I’ve worked in pharma QA for 12 years. The worst offenders? Companies that test at 25°C/60% RH but sell in Nigeria. They think ‘it’s close enough.’ Spoiler: it’s not. I’ve seen kids get sick because a vaccine turned to soup in a Lagos market. This isn’t theory - it’s life or death.
Robb Rice
January 7, 2026 AT 04:22Thanks for the detailed breakdown. One small correction - the ICH zones are technically defined by climate, not just temperature/humidity. Zone III is hot-dry, not just hot. Small detail, but important for compliance. Also, typo: ‘Orthography’ should be ‘orthography’ - lowercase. Just sayin’.
Lawver Stanton
January 8, 2026 AT 22:25Let me tell you about the time I worked at a contract lab that got audited for stability testing. We had one chamber that drifted 1.7°C over 72 hours. The QA guy said, ‘Eh, it’s fine, we’ll just note it.’ They got a 47-page warning letter. The CEO cried. The whole team got fired. And guess what? The drug was fine. But the paperwork wasn’t. Welcome to pharma - where the paper trail matters more than the patient.
Sara Stinnett
January 9, 2026 AT 07:38Oh please. You’re selling this like it’s science. It’s politics. The ICH guidelines were written by big pharma lobbyists who want to delay generics. The ‘significant change’ definition? Vague on purpose. So they can reject any competitor’s product on a technicality. This isn’t about safety - it’s about market control.
linda permata sari
January 9, 2026 AT 07:55As someone from Indonesia, I’ve seen medicines melt in the heat. My grandma’s blood pressure pills turned sticky. She didn’t know they were bad. No one told her. This isn’t just a lab thing - it’s a human thing. Thank you for showing what’s really at stake.
Brandon Boyd
January 10, 2026 AT 09:57This is the kind of post that makes me proud to work in this field. Seriously. You don’t hear enough about the quiet heroes who make sure your meds don’t turn into poison. Keep pushing for better standards - the world needs more people like you.
Branden Temew
January 11, 2026 AT 02:23So we spend millions testing pills in climate chambers… but we still can’t figure out why people forget to take them? Maybe the real stability issue isn’t the drug - it’s the human.
Hanna Spittel
January 12, 2026 AT 11:14⚠️ I know this is all a cover-up. The real reason they test at 40°C? So they can say ‘it passed’ and still sell drugs that degrade at 35°C. Big Pharma knows the heat in your car hits 45°C - but they don’t test that. They’re hiding it. 🕵️♀️💊
Brady K.
January 14, 2026 AT 01:15Let’s not romanticize stability testing. It’s a $20B industry built on fear, compliance theater, and legacy protocols that don’t work for mRNA or gene therapies. AI-driven predictive models are already 80% accurate - but regulators won’t accept them because they can’t ‘see’ the data. We’re using slide rules in the age of quantum computing. Pathetic.
Kayla Kliphardt
January 15, 2026 AT 17:55Wait - so if a company sells globally, do they need to run BOTH 25°C and 30°C long-term tests? Or just the one for the harshest market? I’m trying to figure out cost vs. compliance.
John Chapman
January 16, 2026 AT 17:48YES! Exactly what I was thinking! You nailed it. Running both is ideal, but most companies pick the worst-case scenario - 30°C/65% RH - and call it a day. Saves money, still meets global standards. Just make sure your packaging handles the humidity too. 😊