Your lungs move about 11,000 liters of air every day — so protecting them pays off. This page gathers practical tips and clear facts about the respiratory system: common conditions, when to get help, and simple habits that keep your breathing strong.
The respiratory system includes the airways, lungs, and muscles that make breathing possible. Common problems you’ll see are asthma, chronic obstructive pulmonary disease (COPD), bronchitis, pneumonia, and viral infections like flu or COVID. Symptoms that matter: ongoing cough, wheeze, shortness of breath doing daily tasks, chest tightness, or cough with green or bloody sputum. A single mild cough often isn’t urgent, but patterns and persistence are worth tracking.
Watch for these signs and act fast: sudden severe breathlessness, blue lips or nails, fainting or confusion, high fever with fast breathing, and chest pain that doesn’t go away. If you use inhalers and suddenly need them far more often, that’s a warning. For babies and older adults, look for poor feeding, slowed breathing, or sudden changes in alertness. If any of these happen, call emergency services or get to a clinic right away.
Quit smoking and avoid secondhand smoke — the single biggest change you can make. Get yearly flu shots and stay up to date with COVID and pneumococcal vaccines if you are at higher risk. Improve indoor air: use a HEPA filter, keep humidity in a comfortable range, and avoid strong fumes or sprays.
For people with asthma or COPD, learn inhaler technique. Use a spacer with metered-dose inhalers, take controller meds as prescribed, and rinse your mouth after steroid inhalers to cut the risk of thrush. If you’re prescribed a rescue inhaler, discuss newer SABA-free options with your clinician if they fit your care plan.
Simple breathing exercises help. Try pursed-lip breathing to slow your breath during flare-ups: inhale slowly through your nose two counts, exhale through pursed lips for four counts. Controlled coughing clears mucus: sit forward, take a slow deep breath, hold for two seconds, cough two short huffs. Stay hydrated — thin mucus is easier to clear.
Know when to see a specialist. If symptoms persist despite treatment, ask your doctor for lung function testing (spirometry) or a chest X‑ray. Keep a symptom diary — note triggers, medication use, and peak flow numbers if you have an asthma meter. That record makes clinic visits more useful.
If you want reliable reading, start with trusted medical sites and talk to your healthcare team before changing meds. Small daily steps add up: protect your air, treat problems early, and you’ll keep breathing better for years.
Pulmonary rehab is often underrated — physical therapy plus breathing practice can cut symptoms and improve life for COPD or long COVID. Ask your doctor about rehab programs, smoking-cessation support, and weight or sleep assessments if breathing problems follow. Check daily air quality apps and avoid outdoor activity when alerts are high. Use N95 masks around heavy smoke or pollution. Small, concrete steps like these add big wins to lung health.
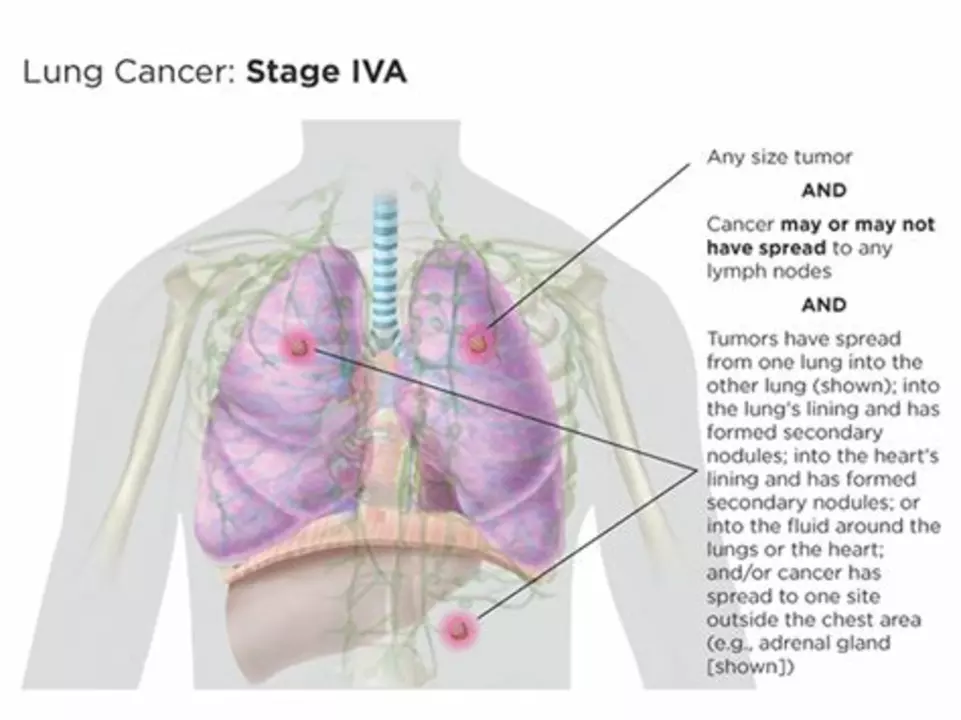
As a blogger, I've recently researched how tumor growth can affect our respiratory system. I discovered that when tumors develop in the lungs, they can obstruct airways and restrict the flow of oxygen in our body. This may cause shortness of breath, coughing, and chest pain, which can significantly impact our daily lives. Additionally, tumors may also invade surrounding tissues or metastasize to other parts of the body, causing further complications. It's crucial to keep an eye on any changes in our respiratory health and consult a doctor if we experience any concerning symptoms.
View more