Topical steroids work - but only if you use them right
Most people think topical steroids are just another cream you slap on a rash and forget about. But that’s where things go wrong. These medications are powerful tools for eczema, psoriasis, and stubborn dermatitis - but they’re not harmless lotions. Used incorrectly, even for a few weeks, they can cause your skin to thin out, bruise easily, or develop stretch marks. And once that damage happens, it doesn’t always come back.
The good news? When used properly, topical steroids are safe, effective, and often life-changing. Millions of people use them every day without issues. The difference isn’t the medicine - it’s how you use it.
What topical steroids actually do
Topical corticosteroids are anti-inflammatory drugs applied directly to the skin. They don’t cure eczema or psoriasis. Instead, they quiet down the immune system’s overreaction that causes redness, itching, and flaking. Unlike oral steroids that flood your whole body, topical versions mostly stay where you put them. Your skin breaks down most of the medicine before it can enter your bloodstream, which is why they’re safer than pills.
They’ve been around since the 1950s and are still the most common prescription for skin inflammation. In the U.S., about 40% of all dermatology prescriptions are for topical steroids. Hydrocortisone, the mildest form, is even available over the counter. But strength matters - a lot.
Potency levels: Not all steroids are created equal
There are seven classes of topical steroids, ranked from super-potent (Class I) to low-potency (Class VII). Think of it like a ladder: the higher you go, the stronger the effect - and the greater the risk if misused.
- Super-potent (Class I): Betamethasone dipropionate, clobetasol. Used only for thick, stubborn plaques on elbows or soles - never on the face.
- High to moderate (Classes II-IV): Mometasone, triamcinolone. Good for moderate eczema on arms, legs, or torso.
- Low-potency (Classes V-VII): Hydrocortisone 1%, desonide. Safe for face, groin, and underarms - and often enough for mild flares.
The vehicle (the base the steroid is mixed into) also changes how strong it feels. Ointments are the most potent because they lock moisture in. Creams are next. Gels and lotions are lighter and better for hairy areas or oily skin. Foams work well on the scalp.
How much to use: The fingertip unit trick
Most people use too little - or way too much. The fix? Learn the fingertip unit (FTU).
One FTU is the amount of cream or ointment you squeeze from a tube onto the last joint of your index finger. It’s not a pea. It’s not a dab. It’s a full line from tip to joint.
Here’s what one FTU covers:
- One hand (front and back): 1 FTU
- One arm (front and back): 3 FTUs
- One leg: 6 FTUs
- One foot: 2 FTUs
- Face and neck: 2.5 FTUs
Studies show patients who get this right see faster results and fewer side effects. If you’re using less than this, you’re prolonging the flare. If you’re using more, you’re risking skin thinning.
How often to apply: Once a day is enough
You don’t need to apply topical steroids twice a day - not even for severe cases. The American Academy of Family Physicians found no benefit to applying them more than once daily. In fact, doing so only increases your risk of side effects without speeding up healing.
Super-potent and moderate steroids should be used once a day. Low-potency ones can go twice a day if your doctor says so. But never go beyond what’s written on the prescription. More doesn’t mean better. It just means more damage.

Where you apply matters more than you think
Your skin isn’t the same everywhere. The face, eyelids, groin, armpits, and breasts have thin skin. That’s why only mild steroids (like hydrocortisone 1%) are approved for those areas. Using a strong steroid on your eyelids for weeks can lead to glaucoma or cataracts. On the face, it can cause acne, red rashes around the mouth (perioral dermatitis), or permanent redness.
Thicker skin - like on your palms, soles, or back - can handle stronger formulations. But even there, don’t use super-potent steroids for more than two weeks without checking in with your doctor.
How long is too long?
There’s no universal rule, but here’s what experts agree on:
- Super-potent steroids: Max 2 weeks
- High-potency steroids: Max 2-4 weeks
- Moderate to low-potency: Up to 6-8 weeks, but only if needed
After that, you need to step down. That means switching to a weaker steroid, using it less often, or switching to a non-steroidal option like tacrolimus or crisaborole. This is called step-down therapy - and it’s the gold standard for chronic conditions like eczema.
Some patients use a strong steroid for 10 days to knock down a flare, then switch to a low-strength one every other day for maintenance. That’s how you control symptoms without wrecking your skin.
What skin thinning looks like
It doesn’t happen overnight. But over time, you’ll notice:
- Skin that looks translucent or paper-thin
- Visible blood vessels (telangiectasia)
- Easily bruised skin, even from light bumps
- Stretch marks that don’t fade
- Slower healing of cuts or scrapes
These signs are most common in areas where skin is naturally thin - armpits, inner thighs, neck, face. But they can show up anywhere if you’ve been overusing strong steroids.
Once skin atrophy sets in, it can take months - sometimes years - to recover. In some cases, it never fully goes back. That’s why prevention is everything.
What to do with moisturizers
Moisturizers aren’t optional - they’re part of the treatment. But applying them right after your steroid? That’s a mistake.
Wait 20 to 30 minutes after applying the steroid before putting on your moisturizer. If you don’t, the cream washes the steroid off or dilutes it, making it less effective. You end up using more of both - and increasing your risk of side effects.
Also, wash your hands before and after applying. Don’t rub the steroid into unaffected skin. Only treat the red, flaky, itchy areas.
What happens when you stop too soon - or too late
Some people panic and quit steroids as soon as the redness fades. That’s a recipe for rebound flares. Others keep using them for months because they feel better. That’s how dependency and atrophy start.
There’s also a condition called topical steroid withdrawal (TSW), where people who used high-potency steroids long-term on sensitive areas suddenly stop - and get intense redness, burning, and itching. It’s rare, but real. And it’s almost always tied to unsupervised, long-term use.
The key is planning your exit. Don’t just quit. Talk to your doctor. Taper slowly. Use a weaker steroid every other day. Then switch to moisturizer only. Your skin needs time to reset.
Alternatives to steroids
Non-steroidal options like tacrolimus (Protopic) and crisaborole (Eucrisa) are growing in popularity - especially for the face and sensitive areas. They don’t cause skin thinning. But they’re more expensive, and not always covered by insurance. Still, for people who’ve had bad reactions to steroids, they’re a game-changer.
They work differently - they block inflammation without suppressing the immune system the same way steroids do. They’re not faster, but they’re safer for long-term use. Many dermatologists now recommend them as maintenance therapy after a steroid flare-up.
Real stories, real consequences
A woman in Cape Town used a strong steroid cream on her face for six months to treat what she thought was acne. When she stopped, her skin turned bright red, burned constantly, and started peeling. She’d developed perioral dermatitis and steroid-induced atrophy. It took 18 months of careful treatment to get her skin back to normal.
Another man used a super-potent steroid on his inner thighs for eczema for over a year. He didn’t realize his skin had thinned until he noticed bruises appearing with no injury. He needed a dermatologist to confirm the damage - and a new treatment plan.
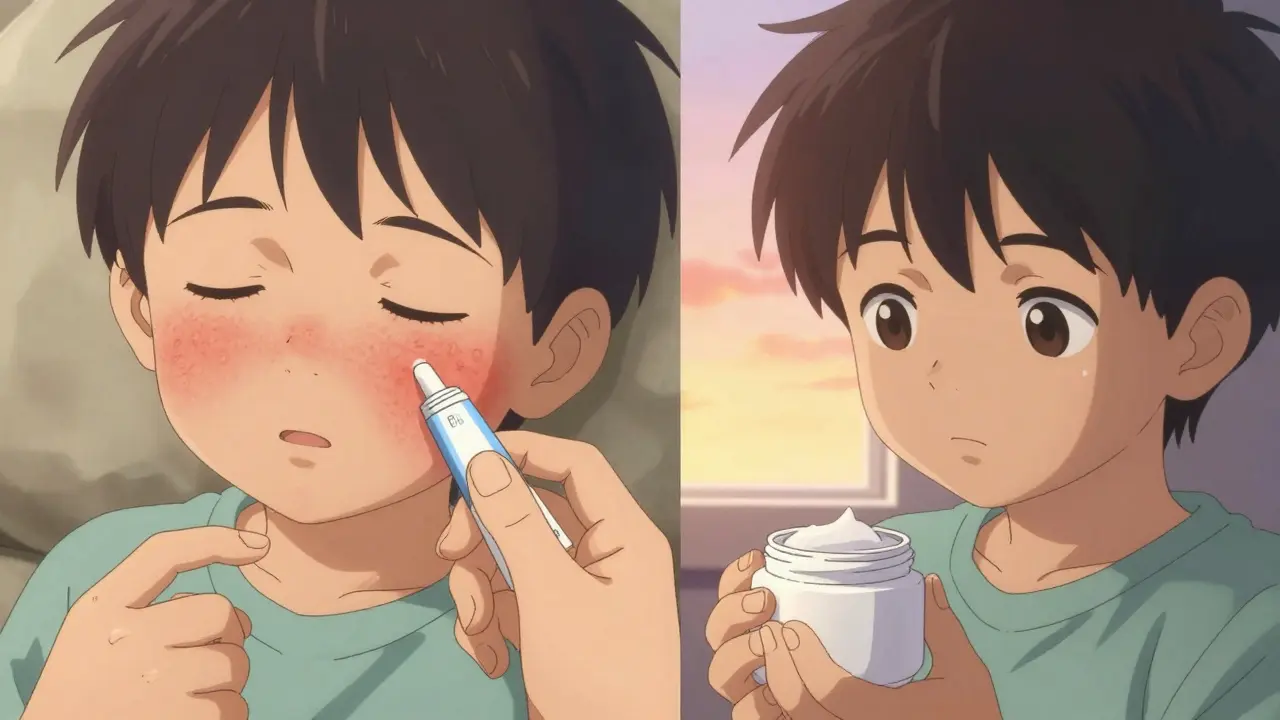
But there are also success stories. A mother in Johannesburg used a step-down plan: strong steroid for 10 days, then a mild one every other day, then just moisturizer. Her child’s eczema stayed under control for over a year without side effects.
The difference? Guidance. Monitoring. Knowing when to stop.
Your action plan: Use steroids smart
- Get the right strength. Don’t use a high-potency steroid unless your doctor says so - and only for thick skin.
- Use FTUs. Measure your dose. Don’t guess.
- Apply once a day. More isn’t better.
- Never use strong steroids on the face, eyelids, or groin. Stick to hydrocortisone 1% there.
- Limit use to 2-4 weeks. After that, step down or switch.
- Wait 30 minutes before moisturizing. Don’t mix them.
- Watch for thinning. If skin looks see-through, bruises easily, or shows stretch marks - stop and see a doctor.
- Plan your exit. Don’t quit cold turkey. Taper slowly with your doctor’s help.
Bottom line
Topical steroids aren’t dangerous. They’re just powerful. Like a knife - useful in skilled hands, risky in untrained ones. The key isn’t avoiding them. It’s using them with intention, precision, and respect.
If you’ve been using a steroid for longer than a month without a check-in, it’s time to talk to your doctor. If you’re unsure how much to use, ask for a demonstration. If your skin looks different - thinner, redder, more bruised - don’t ignore it.
These medications saved millions of lives. But they won’t save you if you use them wrong.
Can topical steroids cause permanent skin damage?
Yes, but only with long-term misuse. Skin thinning (atrophy), visible blood vessels, and stretch marks can become permanent if strong steroids are used daily for months on thin skin areas like the face or groin. The good news? If caught early and stopped, many changes can improve over time - sometimes fully. But the longer you wait, the less likely full recovery becomes.
Is hydrocortisone cream safe for long-term use?
Hydrocortisone 1% (low-potency) is generally safe for daily use on sensitive areas for up to 4-6 weeks. But even mild steroids shouldn’t be used continuously for months without medical supervision. For chronic conditions like eczema, doctors recommend using it only during flares, then switching to moisturizers or non-steroidal creams for maintenance.
Can I use topical steroids on my child’s face?
Only mild steroids like hydrocortisone 1% should be used on a child’s face - and only for short periods (up to 1-2 weeks). Never use medium or high-potency steroids on the face, even if the rash looks bad. Children’s skin is thinner and more absorbent, making them more vulnerable to side effects like skin thinning or hormonal changes.
Why does my skin get worse after I stop using the steroid?
This is called rebound flare or topical steroid withdrawal. It usually happens after long-term use (months) of high-potency steroids, especially on the face or genitals. Your skin becomes dependent on the steroid to suppress inflammation. When you stop, the immune system reacts strongly, causing redness, burning, and itching. The solution is slow tapering - not sudden stopping - under a doctor’s care.
Are there natural alternatives to topical steroids?
There’s no true natural replacement that works as well as steroids for inflammation. Some people try coconut oil, aloe vera, or colloidal oatmeal - and these can help soothe mild irritation. But they don’t stop the immune response like steroids do. For moderate to severe eczema or psoriasis, non-steroidal prescription options like tacrolimus or crisaborole are the best alternatives - not home remedies.
How do I know if I’m using too much?
You’re using too much if you’re going through a tube in less than two weeks for a small area, or if your skin looks shiny, thin, or bruised. Also, if you’re applying it to areas that aren’t inflamed - like healthy skin around a rash - you’re overdoing it. Stick to the fingertip unit rule: one FTU per body part, once daily. Less is more.


Laia Freeman
January 29, 2026 AT 00:48rajaneesh s rajan
January 30, 2026 AT 22:02paul walker
February 1, 2026 AT 11:19Alex Flores Gomez
February 3, 2026 AT 04:38Frank Declemij
February 4, 2026 AT 15:42Pawan Kumar
February 6, 2026 AT 08:29Keith Oliver
February 7, 2026 AT 15:03Kacey Yates
February 9, 2026 AT 08:53ryan Sifontes
February 11, 2026 AT 05:01Jasneet Minhas
February 11, 2026 AT 08:27Megan Brooks
February 12, 2026 AT 12:48Robin Keith
February 14, 2026 AT 02:44Sheryl Dhlamini
February 15, 2026 AT 04:09