When you pick up a prescription, brand dispensing, the practice of giving a name-brand drug instead of a cheaper generic version, even when the generic is approved and available. Also known as name-brand dispensing, it happens when a prescriber writes "Do Not Substitute" or when the pharmacy chooses to dispense the brand for reasons like patient history, insurance rules, or perceived reliability. This isn’t just a pharmacy quirk—it directly affects how much you pay, how quickly you get your meds, and even whether you stick with your treatment plan.
Many people assume generics are just cheaper versions of the same drug. They are—but that doesn’t mean they’re less effective. The FDA and Health Canada require generics to have the same active ingredient, strength, and absorption rate as the brand. Still, generic substitution, the process of replacing a brand-name drug with a bioequivalent generic. Also known as therapeutic substitution, it’s a standard part of modern pharmacy practice and saves patients and the system millions every year. But brand dispensing can block that savings. Why? Sometimes it’s because the doctor wrote a non-substitutable script. Other times, it’s because the pharmacy didn’t ask if you’d prefer the cheaper option. And in some cases, insurance plans push brand drugs to get rebates from manufacturers—putting profit ahead of your cost.
It’s not all bad. For some people, brand drugs are the only option that works. A few patients report different side effects or inconsistent results with generics, especially with narrow-therapeutic-index drugs like warfarin or thyroid meds. In those cases, brand dispensing makes sense. But for most common meds—antibiotics, blood pressure pills, antidepressants—the generic is just as safe and just as effective. The real issue? Most patients don’t know they have a choice. Pharmacists are trained to ask, but they won’t push if you don’t speak up. And if your doctor doesn’t mention it, you might pay hundreds extra a year without realizing it.
That’s why the posts below matter. You’ll find real-world guides on how to talk to your pharmacist about generics, how to spot when brand dispensing is unnecessary, and how to challenge a prescription that’s costing you more than it should. You’ll see how pharmacy consultation, a service where pharmacists review your meds to catch errors, interactions, or cost-saving opportunities. Also known as medication review, it’s often free and can prevent costly mistakes helps you avoid overpaying. You’ll learn how prescriber communication, the exchange between doctors and pharmacists about drug choices, substitutions, and patient needs. Also known as pharmacist-prescriber collaboration, it’s the backbone of safe, affordable care can change what ends up in your bottle. And you’ll see how medication costs, the out-of-pocket price you pay for drugs, which can vary wildly depending on brand, insurance, and pharmacy. Also known as drug pricing, it’s a hidden stress point for millions of Canadians don’t have to be a surprise.
These aren’t theoretical debates. They’re daily decisions that affect your health and your budget. The posts here give you the tools to understand when brand dispensing helps—and when it’s just costing you money. You’ll walk away knowing how to ask the right questions, how to read your prescription label, and how to make sure you’re getting the best value without sacrificing safety. What you find below isn’t just information—it’s power.
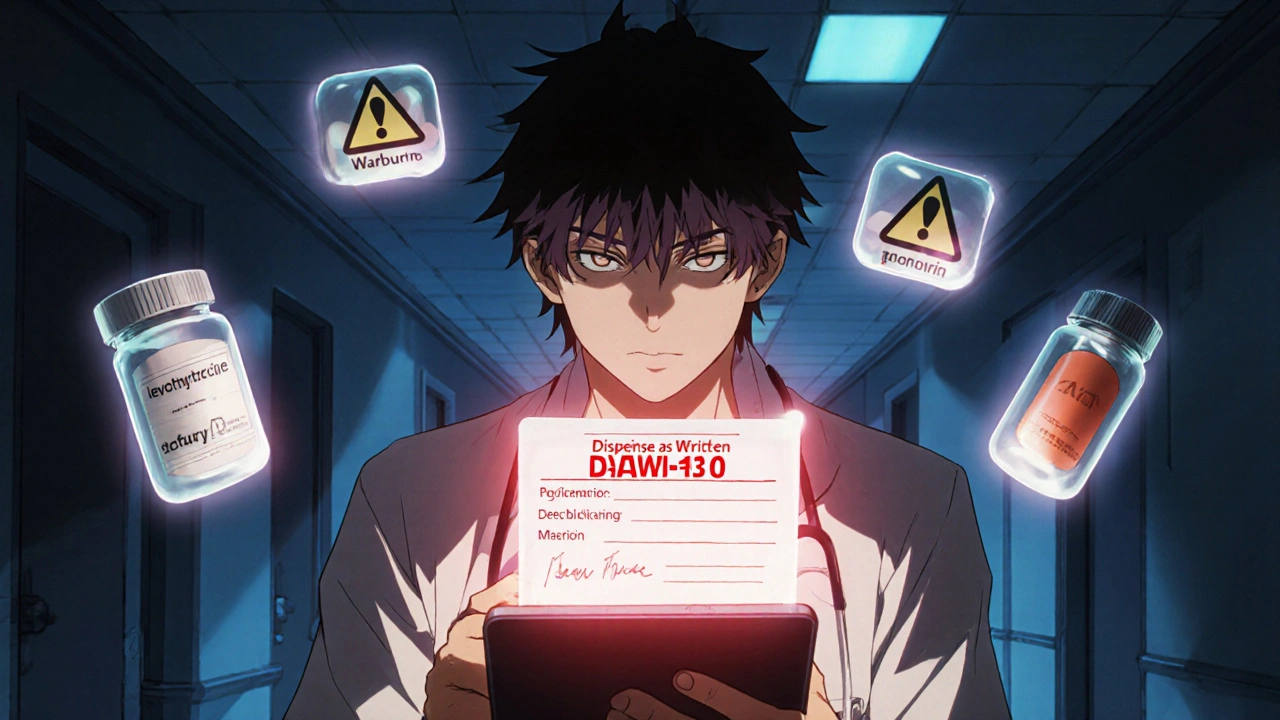
Prescriber override lets doctors require brand-name drugs instead of generics when safety is at risk. Learn how DAW-1 codes, state laws, and EHR systems affect patient safety-and how to use this tool correctly.
View more