When a doctor ignores a warning in the electronic system and still prescribes a drug—despite risks like dangerous interactions or wrong dosing—that’s a prescriber override, a deliberate choice by a clinician to bypass automated safety alerts in electronic prescribing systems. Also known as a clinical override, it’s not a mistake—it’s a decision, often made under pressure, with patient needs in mind.
These overrides aren’t random. They happen when a patient’s history doesn’t fit the system’s rules. Maybe they’ve taken the same drug for years without issue, or their condition needs a medication flagged as high-risk. Systems warn about mixing blood thinners with NSAIDs, but what if the patient has severe arthritis and no other option? Or when a pharmacist flags a drug interaction, but the doctor knows the patient’s liver processes it differently? That’s where prescriber override becomes part of real-world care. It’s not about ignoring safety—it’s about adapting it. The same systems that prevent errors can also block necessary treatments if they’re too rigid. That’s why many hospitals track override rates: too many signals broken rules; too few might mean dangerous drugs are being withheld.
Related to this are pharmacy systems, the digital tools that flag potential errors before a prescription is filled. These systems pull from databases of drug interactions, allergies, and dosing limits. But they don’t know everything. They don’t know if a patient’s rash last year was truly an allergy, or if the ‘high-alert’ medication was the only thing that worked after three others failed. That’s where medication safety, the practice of preventing harm from drugs through careful prescribing, dispensing, and monitoring comes in. It’s not just about alerts—it’s about judgment. And that’s why posts here cover everything from verbal prescriptions and pharmacist consultations to how aging changes drug responses. These aren’t just technical topics—they’re about the human choices behind every prescription.
What you’ll find below are real stories and practical guides from clinicians and patients who’ve dealt with overrides, system errors, and the fine line between safety and necessity. Some posts show how a simple chat with a pharmacist prevented a dangerous mix. Others explain why a doctor chose to override a warning for an elderly patient with kidney issues. You’ll see how temperature control, inhaler technique, and even vitamin K intake tie into the bigger picture: getting the right drug to the right person, at the right time—even when the system says no.
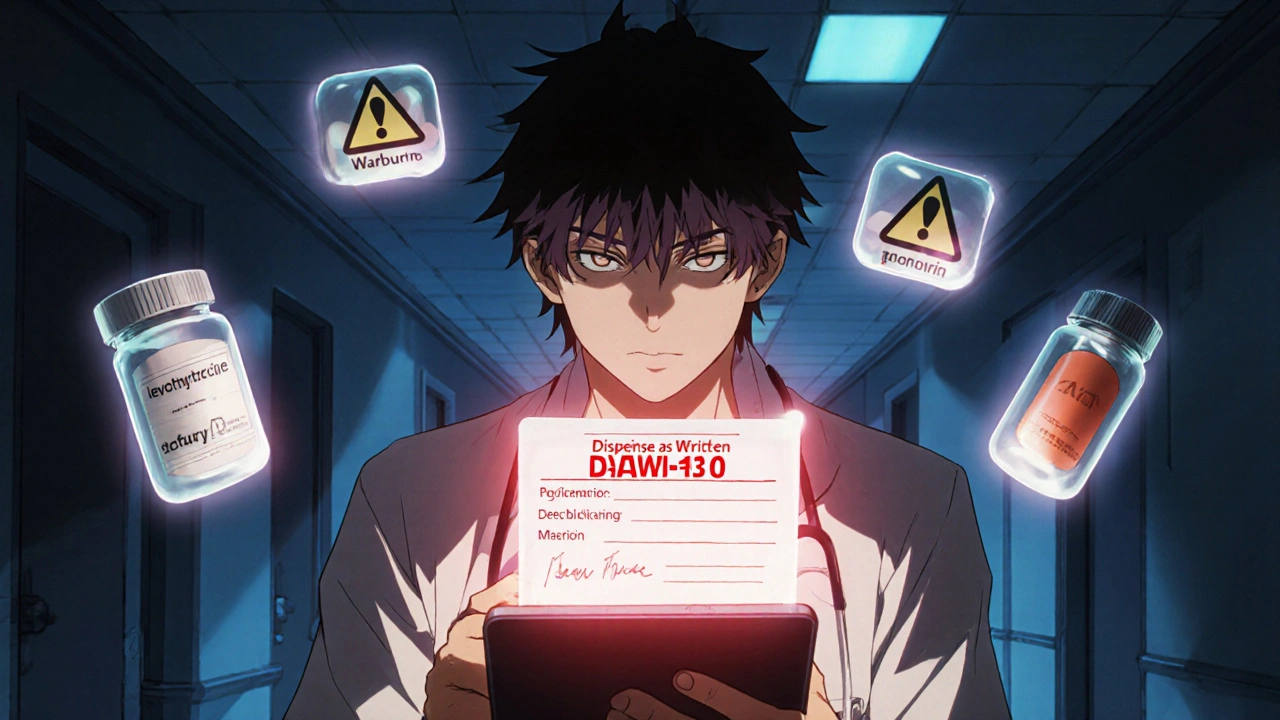
Prescriber override lets doctors require brand-name drugs instead of generics when safety is at risk. Learn how DAW-1 codes, state laws, and EHR systems affect patient safety-and how to use this tool correctly.
View more