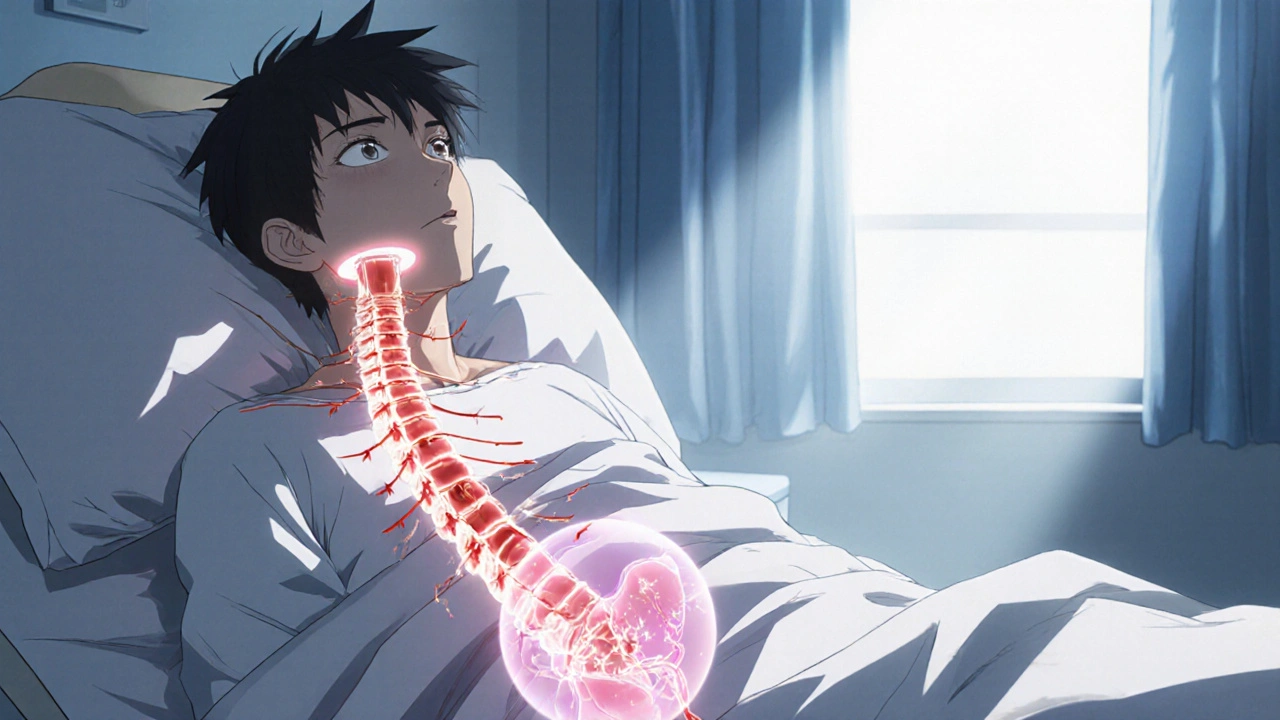
When talking about SCI symptoms, the physical signs that appear after a spinal cord injury (SCI). Also known as spinal cord injury symptoms, they can range from loss of sensation to life‑threatening autonomic events. A spinal cord injury, damage to the spinal cord that disrupts motor, sensory, and autonomic pathways often triggers a cascade of issues. One of the most common complaints is neuropathic pain, a chronic burning or stabbing sensation caused by nerve damage. Another serious manifestation is autonomic dysreflexia, a sudden spike in blood pressure triggered by overstimulation below the injury level. Even routine bodily functions can be altered; for example, bladder dysfunction, loss of bladder control or retention affects up to 80% of people with an SCI. Understanding these entities helps you spot warning signs early and plan appropriate care.
SCI symptoms encompass motor weakness, sensory loss, and autonomic disturbances. Motor weakness often leads to mobility impairment, making everyday tasks like dressing or cooking a challenge. Sensory loss isn’t just numbness; it can hide injuries such as pressure sores, which are a leading cause of hospitalization for people with an SCI. Autonomic issues like temperature regulation problems and sweating irregularities stem from the same nerve pathways that control heart rate and digestion. The relationship between spinal cord injury and autonomic dysreflexia is clear: the injury blocks normal reflex arcs, so even a simple bladder fill can trigger a dangerous blood pressure surge. This cascade illustrates the semantic triple “Spinal cord injury often leads to autonomic dysreflexia.” Likewise, “Neuropathic pain is a frequent component of SCI symptoms” and “Bladder dysfunction frequently follows spinal cord injury” are other triples that map the cause‑effect web.
Management strategies differ by symptom type. For neuropathic pain, clinicians may prescribe gabapentinoids, tricyclic antidepressants, or topical agents, tailoring doses to the individual's pain profile. Autonomic dysreflexia requires rapid blood pressure control—often with sitting the patient upright, removing triggering stimuli, and using fast‑acting antihypertensives if needed. Bladder management ranges from intermittent catheterization to pharmacologic agents that relax the bladder neck. Each approach reflects the underlying physiology: the same damaged pathways that cause loss of movement also drive the autonomic spikes. Recognizing this link helps caregivers choose interventions that address multiple symptoms at once.
Below you’ll discover a curated collection of articles that explore these topics in depth. From dosing guides for drugs that treat neuropathic pain to practical tips for handling fluid retention, the posts cover the full spectrum of SCI‑related challenges. Whether you’re a patient, a family member, or a health professional, the resources aim to give you actionable insight and up‑to‑date information. Dive in to see how each symptom group is addressed, compare treatment options, and find real‑world advice you can apply right away.
Explore how spinal cord injuries disrupt bladder control, cause different types of urinary incontinence, and what diagnostic and treatment options help restore function.
View more