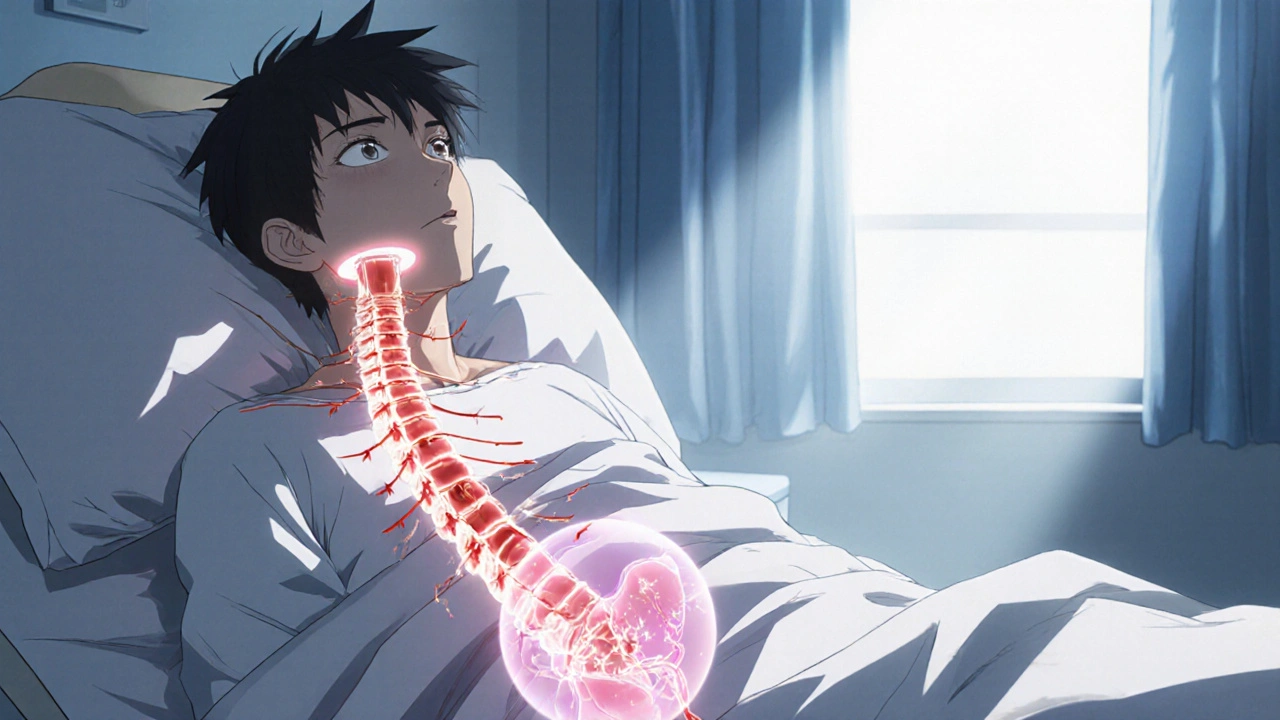
When dealing with spinal cord injury, a traumatic or non‑traumatic disruption of the spinal cord that impairs motor, sensory and autonomic functions. Also known as SCI, it demands immediate medical attention and long‑term multidisciplinary care. Understanding the condition helps you plan for the many challenges that follow.
Effective rehabilitation, a structured program of physical, occupational and speech therapies aimed at restoring function is the cornerstone of recovery. Rehabilitation connects directly to the need for mobility devices, assistive equipment such as wheelchairs, exoskeletons or adaptive seating that enable independence. Together they form a loop: spinal cord injury requires rehabilitation, and rehabilitation leverages mobility devices to improve daily living.
One of the most stubborn complications is neuropathic pain, chronic pain caused by nerve damage that often follows spinal cord injury. This pain influences quality of life, limits participation in therapy, and can derail progress if not managed properly. Addressing neuropathic pain usually involves medication, nerve blocks, and targeted physiotherapy, all coordinated within the rehabilitation plan.
Autonomic functions are equally critical. Bladder management, strategies ranging from intermittent catheterization to pharmacologic control, is essential for health and social confidence. Proper bladder care reduces infection risk, prevents renal damage, and supports a smoother transition back to community life.
Beyond the core areas mentioned, spinal cord injury also interacts with respiratory support, mental health, and vocational reintegration. Each of these facets creates a network of needs that clinicians, caregivers, and patients must navigate. For example, respiratory therapy often goes hand‑in‑hand with early rehabilitation to prevent pneumonia, while counseling helps address the emotional shock of sudden disability.
Understanding the cascade of effects helps you make better choices. When you know that spinal cord injury can lead to secondary conditions like pressure ulcers, you’ll prioritize skin checks and proper seating. Knowing the link between neuropathic pain and sleep disturbances guides you to look for both pain relief and sleep hygiene strategies.
The posts below dive into specific medications, treatment comparisons, and practical tips that tie directly into the themes we’ve outlined. Whether you’re searching for the latest drug comparison for managing pain, looking for advice on fluid retention that can affect edema, or curious about how certain medications might impact bone health, you’ll find a curated set of resources that address the real‑world questions that arise after a spinal cord injury.
Browse the collection to see detailed guides on medication safety, dosing strategies, and lifestyle adjustments that complement the rehabilitation journey. Each article is written to give you actionable information you can discuss with your health team.
Now that you have a solid overview of the main challenges and the tools to tackle them, explore the individual posts to deepen your understanding and find the specific guidance you need for your situation.
Explore how spinal cord injuries disrupt bladder control, cause different types of urinary incontinence, and what diagnostic and treatment options help restore function.
View more