When you pick up a prescription, you might see a different name on the bottle than what your doctor wrote. That’s often because the pharmacy substituted it with a therapeutic equivalence, the official standard that says two drugs work the same way in the body, even if they’re made by different companies. Also known as bioequivalence, it’s the reason your $15 generic pill can replace a $150 brand-name one without losing effectiveness. But therapeutic equivalence isn’t just a label—it’s a safety net. It means your body absorbs the drug the same way, hits the same blood levels, and gives you the same results. If two drugs aren’t therapeutically equivalent, switching them could mean your condition gets worse—or you get side effects you didn’t expect.
Not every drug has this guarantee. For most pills like antibiotics, blood pressure meds, or antidepressants, the FDA requires strict testing to prove therapeutic equivalence. But for complex drugs like biologics, injectables, or extended-release formulas, the rules get fuzzy. That’s why you’ll see posts here about biologic therapies, high-cost, protein-based treatments for autoimmune and cancer conditions and why injecting them safely matters. Or why therapeutic drug monitoring, the process of checking blood levels to make sure a drug is working right and not too high is critical for tricyclic antidepressants or digoxin. These aren’t simple generics. They need careful tracking because small differences can have big consequences.
Therapeutic equivalence also affects how your body handles aging. Seniors often take multiple meds, and switching to a generic without checking for equivalence can throw off their whole regimen. That’s why posts on elderly medication safety, how older adults process drugs differently due to slower metabolism and kidney changes are so important. A generic version of a drug might look the same, but if it’s absorbed faster or slower, it could cause dizziness, falls, or confusion in someone over 70. Even something as simple as medication storage, keeping pills at the right temperature and humidity to preserve their strength ties into this. A pill that degrades because it was shipped in a hot truck might still be labeled as therapeutically equivalent—but it won’t work like it should.
You’ll find posts here that dig into real-world examples: how to compare Premarin with estradiol patches, why Ecosprin (aspirin) might be safer than ibuprofen for some, or why switching from Dilantin to a newer seizure drug needs caution. Some of these aren’t about generics at all—they’re about knowing when a drug is truly interchangeable, and when it’s not. Whether you’re managing diabetes, depression, or heart rhythm issues, therapeutic equivalence is the quiet rule that keeps your treatment on track. But it’s not foolproof. That’s why understanding it matters. Below, you’ll find practical guides that show you exactly how to spot safe swaps, avoid hidden risks, and talk to your pharmacist or doctor about what really works for your body.

Authorized generics are the exact same medication as brand-name drugs, made by the same company with identical ingredients. They offer the same effectiveness at a lower cost-no compromises.
View more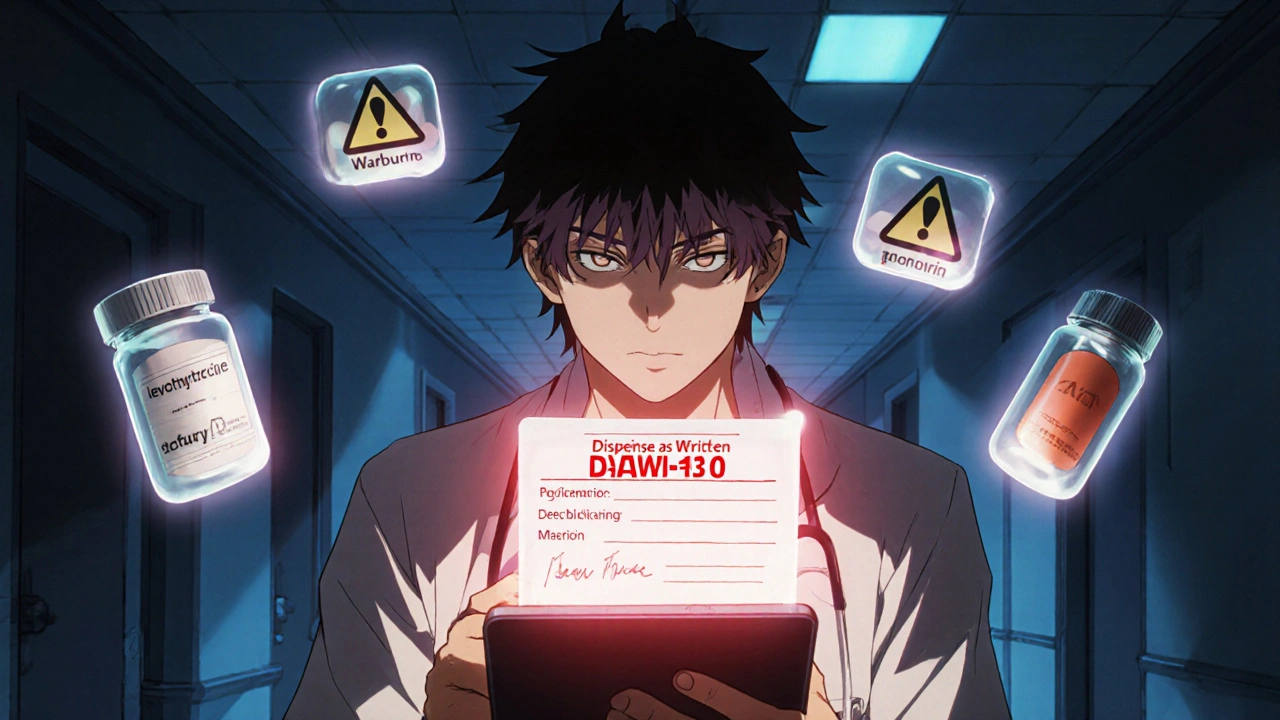
Prescriber override lets doctors require brand-name drugs instead of generics when safety is at risk. Learn how DAW-1 codes, state laws, and EHR systems affect patient safety-and how to use this tool correctly.
View more
Pharmacists play a key role in recommending generic drugs to prescribers, using FDA data to ensure safety, efficacy, and cost savings. Learn how communication, regulations, and evidence drive generic substitution in modern pharmacy practice.
View more