When dealing with Urinary Incontinence, the involuntary leakage of urine that impacts millions of adults. Also known as bladder leakage, it can stem from weak pelvic muscles, nerve issues, or an enlarged prostate. Understanding the condition starts with recognizing that urinary incontinence includes stress, urge, and overflow types, each with its own trigger and treatment pathway.
One major player in male bladder health is Benign Prostatic Hyperplasia (BPH), a non‑cancerous enlargement of the prostate gland that narrows the urethra. BPH often pushes on the bladder, causing urgency and occasional leakage, making it a frequent companion of urinary incontinence. Managing BPH with medication or surgery can directly lower incontinence episodes, illustrating how prostate health influences bladder control.
Medication choices also matter. Diuretics, drugs that increase urine output to reduce fluid buildup are prescribed for hypertension and edema, but they can unintentionally worsen leakage if not timed correctly. Pairing diuretics with scheduled voiding or pelvic floor training helps balance fluid removal with bladder capacity, showing the link between drug therapy and incontinence management.
Beyond pills, Fluid Retention, the accumulation of excess water in tissues that can cause swelling and swelling‑related urine urgency plays a hidden role. When the body holds onto fluid, the kidneys eventually dump it, increasing nighttime trips to the bathroom and raising the risk of accidental leaks. Simple lifestyle tweaks—like reducing salty foods and raising the legs—can cut retention, easing pressure on the bladder.
Effective treatment often blends several approaches. Pelvic floor muscle exercises (Kegels) strengthen the muscles that close the urethra, directly combating stress leakage. Behavioral strategies such as bladder training teach the brain to hold urine longer, targeting urge incontinence. For more severe cases, doctors may recommend medications that relax the bladder or surgical options that support urethral closure. Each option reflects a different angle of the same problem: restoring control over bladder emptying.
When you combine these insights, a clear picture emerges: urinary incontinence is not a single issue but a network of factors—prostate size, drug regimens, fluid balance, and muscle strength. Recognizing these connections lets you choose the right mix of lifestyle changes, exercises, and medical interventions. Remember, the goal isn’t just to stop leaks; it’s to improve overall quality of life, sleep better, and feel confident in daily activities.
The articles that follow dive deeper into each of these areas. You’ll read about specific diabetes meds that affect bladder function, side‑by‑side antibiotic comparisons that matter for infection‑related leakage, and practical tips to reduce fluid retention fast. There are also guides on diuretic choices, BPH symptom management, and exercises to boost pelvic strength. Each piece is chosen to give you actionable advice, whether you’re looking for medical details or simple home‑based solutions. Let’s explore the range of information that can help you take control of urinary incontinence.
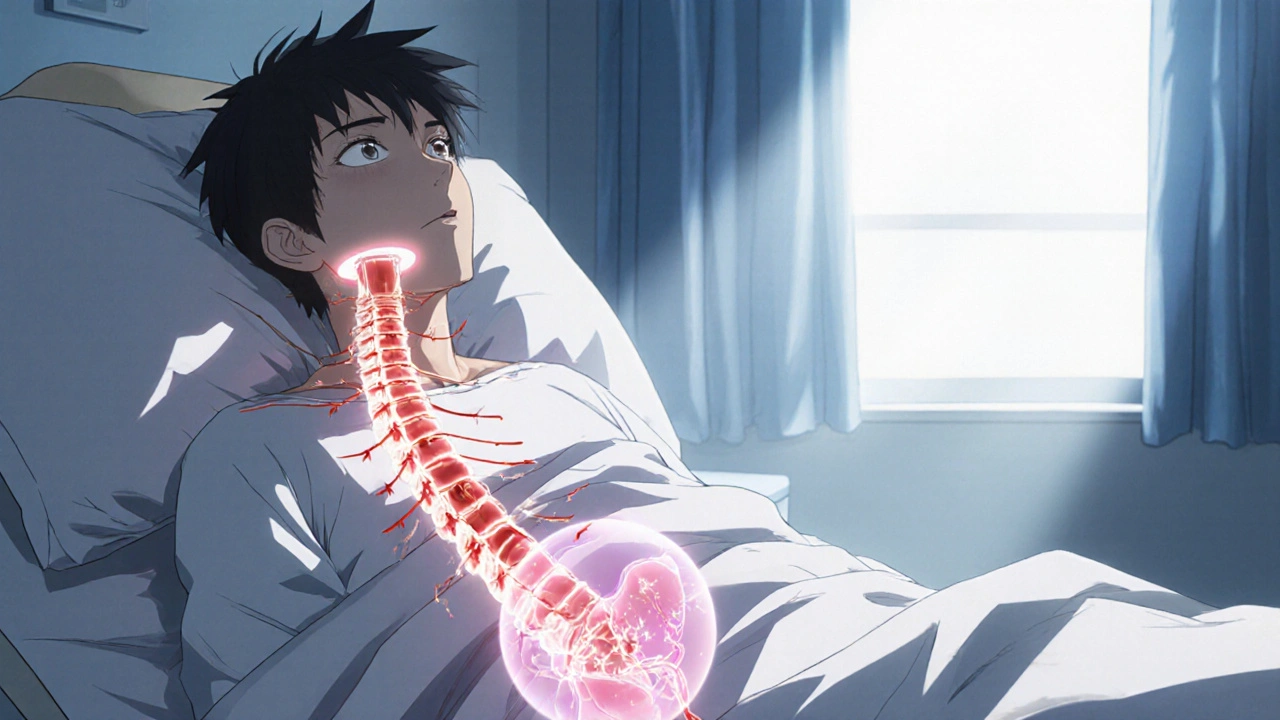
Explore how spinal cord injuries disrupt bladder control, cause different types of urinary incontinence, and what diagnostic and treatment options help restore function.
View more